A client who has been taking benzodiazepine sedative every night for two weeks wishes to stop taking them now. The nurse advises the client to:
continue taking the sedative and discuss slowly decreasing the dose with the physician.
take the last pill on a Friday so that extra sleep can be obtained on the weekend.
continue to take the pills since sleeping without them will be very difficult.
stop taking the medication and take an antihistamine instead.
The Correct Answer is A
A. Gradual tapering of benzodiazepines under medical supervision is recommended to minimize withdrawal symptoms and rebound insomnia. The client should continue taking the medication as prescribed while discussing a tapering plan with their physician.
B. Abruptly stopping benzodiazepines can lead to withdrawal symptoms, including rebound insomnia, anxiety, agitation, and even seizures. Planning to stop medication on a specific day without medical guidance can increase the risk of withdrawal symptoms occurring during the workweek.
C. While it may be challenging to sleep without benzodiazepines initially, continued use can lead to dependence and tolerance, making it even more challenging to discontinue them in the future. Gradual tapering under medical supervision is the preferred approach.
D. Antihistamines are not typically used as substitutes for benzodiazepines in managing insomnia. Additionally, abruptly stopping benzodiazepines and switching to another medication without medical guidance can lead to withdrawal symptoms and inadequate management of insomnia.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
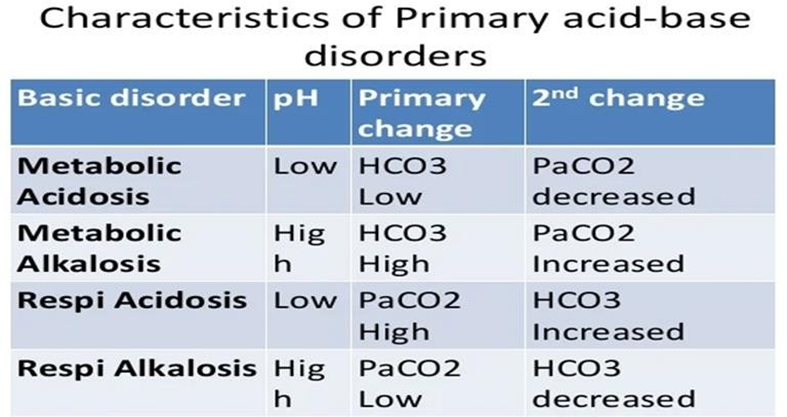
D. In metabolic acidosis, the pH would be low (acidemic) and the HCO3 level would be below the normal range. In the provided ABG results, the pH is low (acidemic) and the HCO3 level is below the normal range, indicating metabolic acidosis.
A. In respiratory alkalosis, the pH would be elevated (alkalotic) and the PaCO2 would be below the normal range (hypocapnia). However, in the provided ABG results, the pH is low (acidemia) rather than high, ruling out respiratory alkalosis.
B. In respiratory acidosis, the pH would be low (acidemic) and the PaCO2 would be above the normal range (hypercapnia). However, in the provided ABG results, the PaCO2 is within the normal range, ruling out respiratory acidosis.
C. In metabolic alkalosis, the pH would be elevated (alkalotic) and the HCO3 level would be above the normal range. However, in the provided ABG results, the pH is low (acidemic) and the HCO3 level is below the normal range, ruling out metabolic alkalosis.
Correct Answer is B
Explanation
B. This client's excitement to learn about a new prosthesis indicates a positive attitude towards rehabilitation and a willingness to engage in the learning process. Their enthusiasm suggests a high level of motivation to adapt to their new prosthesis and incorporate it into their daily life. Therefore, this client exhibits a high motivation to learn.
A. This client's struggle with following nursing directives regarding discharge goals suggests a lack of motivation or difficulty engaging in the rehabilitation process. They may be experiencing challenges or barriers that are impeding their progress. Therefore, they do not exhibit the highest motivation to learn at this time.
C. While this client may have valuable experience and insights to share with newcomers, being a "coach" does not necessarily indicate a high motivation to learn for themselves. While they may be motivated to help others, it doesn't necessarily reflect their own eagerness to engage in learning activities for their own rehabilitation goals.
D. This client's eagerness to be discharged may suggest a desire to move on from the rehabilitation facility rather than a motivation to engage in learning activities related to their rehabilitation. They may be more focused on the end goal of leaving the facility rather than actively participating in the rehabilitation process.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
