A client who is reaching saturation with medication reports the onset of muscle soreness and fatigue, and the practical nurse (PN) notes that the client's skin is warm to the touch.
Which action by the PN is a priority?
Administer a PRN dose of acetaminophen.
Encourage the client to drink fluids.
Report the findings to the charge nurse.
Monitor the client's serum lipid levels.
The Correct Answer is C
This is the priority action by the practical nurse (PN) because it can help identify and prevent a potential adverse reaction to the medication. A client who is reaching saturation with medication means that the client has reached the maximum level of medication in the blood that can produce the desired therapeutic effect. However, this also means that the client is at a higher risk of developing toxicity or side effects from the medication. The PN should report the findings of muscle soreness, fatigue, and warm skin to the charge nurse, as these may indicate signs of inflammation, infection, or allergic reaction to the medication. The PN should also monitor the client's vital signs, oxygen saturation, and laboratory values, and document the findings. The charge nurse should notify the health care provider and adjust the medication dosage or regimen as ordered.
a) Administer a PRN dose of acetaminophen.
This is not the priority action by the PN because it does not address the underlying cause of the client's symptoms. Acetaminophen is an analgesic and antipyretic medication that can help reduce pain and fever. However, it does not treat inflammation, infection, or allergy, which may be the reasons for the client's muscle soreness, fatigue, and warm skin. The PN should administer a PRN dose of acetaminophen only after reporting the findings to the charge nurse and obtaining an order from the health care provider.
b) Encourage the client to drink fluids.
This is not the priority action by the PN because it does not address the underlying cause of the client's symptoms. Drinking fluids can help maintain hydration and electrolyte balance in the body, which are important for normal functioning of cells and organs. However, it does not treat inflammation, infection, or allergy, which may be the reasons for the client's muscle soreness, fatigue, and warm skin. The PN should encourage the client to drink fluids only after reporting the findings to the charge nurse and obtaining an order from the health care provider.
d) Monitor the client's serum lipid levels.
This is not the priority action by the PN because it is not related to the client's symptoms. Serum lipid levels are measures of fats and cholesterol in the blood, which are important for energy production, hormone synthesis, and cell membrane structure. However, they are not related to inflammation, infection, or allergy, which may be the reasons for the client's muscle soreness, fatigue, and warm skin. The PN should monitor the client's serum lipid levels only if they are prescribed a medication that can affect lipid metabolism, such as statins or fibrates.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
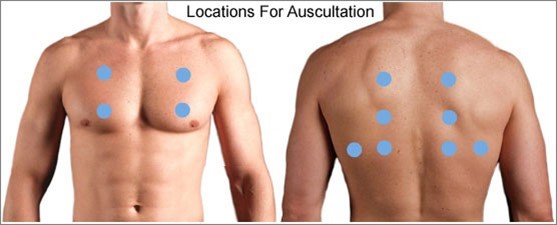
When assessing an older client with left-sided heart failure (HF), the most important intervention for the practical nurse (PN) to implement is to auscultate all lung fields. Left-sided heart failure is characterized by the inability of the left ventricle to effectively pump blood, leading to fluid accumulation in the lungs. Auscultating all lung fields allows the PN to assess for the presence of abnormal lung sounds such as crackles, indicating pulmonary congestion.
Let's evaluate the other options:
a) Inspect for sacral edema.
Sacral edema is commonly associated with right-sided heart failure, not left-sided heart failure. While it is important to assess for edema in clients with heart failure, inspecting for sacral edema may not be the most immediate and crucial intervention in this specific case.
b) Measure urinary output.
Measuring urinary output is a valuable assessment in many clinical situations, but it may not be the most vital intervention in the context of left-sided heart failure. Monitoring urinary output is more relevant in assessing kidney function and fluid balance rather than directly assessing the severity of left-sided heart failure.
d) Check mental acuity.
Checking mental acuity is important in assessing the overall condition of the client, but it is not the most crucial intervention specifically related to left-sided heart failure. Mental status evaluation is more useful in identifying signs of altered mental status or potential complications, rather than directly assessing the impact of left-sided heart failure.
In summary, when assessing an older client with left-sided heart failure, the most important intervention for the practical nurse (PN) to implement is to auscultate all lung fields. This allows for the detection of abnormal lung sounds associated with pulmonary congestion, a hallmark sign of left-sided heart failure.
Correct Answer is ["A","D","E"]
Explanation
Choice A rationale:
Correcting electrolytes that are out of normal range is a crucial goal of therapy for this client. In diabetic ketoacidosis (DKA), the body’s cells are unable to use glucose for energy due to a lack of insulin. This leads to the breakdown of fat for energy, producing ketones as a by-product. Ketones are acidic and can cause the blood’s pH to decrease, leading to metabolic acidosis. This process also leads to an increased production and excretion of electrolytes such as potassium and sodium. Therefore, correcting these electrolyte imbalances is a key goal of therapy.
Choice B rationale:
While promoting oxygenation to tissues is generally important in critical care, it is not a specific goal in the management of DKA. The primary issues in DKA are metabolic in nature, including hyperglycemia, ketosis, and acidosis.
Choice C rationale:
Preventing hyperventilation is not a specific goal in the management of DKA. Hyperventilation in DKA is a compensatory mechanism for metabolic acidosis (Kussmaul breathing). The body tries to expel more carbon dioxide to reduce the acidity of the blood.
Choice D rationale:
Reversing dehydration is another important goal of therapy for this client. In DKA, high blood glucose levels lead to osmotic diuresis, where water is drawn into the urine from the blood, leading to dehydration. This can cause hypotension and reduced tissue perfusion. Therefore, reversing dehydration through fluid replacement is a key part of treatment.
Choice E rationale:
Replacing insulin is a fundamental goal of therapy for this client. Insulin deficiency is the primary cause of DKA. Insulin allows glucose to enter cells where it can be used for energy, preventing the breakdown of fat for energy and the subsequent production of ketones.
Choice F rationale:
Providing respiratory support may be necessary in severe cases of DKA where the patient’s compensatory respiratory efforts are insufficient to maintain adequate gas exchange. However, it is not one of the primary goals of therapy in DKA management.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
