A nurse is caring for a child who has cystic fibrosis and requires postural drainage.
Which of the following actions should the nurse take?
Hold hand flat to perform percussions on the child.
Perform the procedure twice each d
Perform the procedure prior to meals.
Administer a bronchodilator after the procedure
The Correct Answer is C
The correct answer is choice C. Perform the procedure prior to meals.
This is because postural drainage involves positioning the child in different ways to help drain the mucus from the lungs.
If the child has a full stomach, this can cause nausea, vomiting, or aspiration. Therefore, the nurse should perform the procedure before meals or at least 1 hour after meals.
Choice A is wrong because the nurse should not hold the hand flat to perform percussions on the child.
Percussions are rhythmic clapping on the chest wall to loosen the mucus. The nurse should use a cupped hand to create a small air pocket that enhances the vibrations and prevents bruising.
Choice B is wrong because the nurse should not perform the procedure twice a day. The recommended frequency of postural drainage is 3 to 4 times a day, or more if needed, depending on the child’s condition and tolerance.
Choice D is wrong because the nurse should not administer a bronchodilator after the procedure.
A bronchodilator is a medication that relaxes and widens the airways, making it easier to breathe. The nurse should administer a bronchodilator before the procedure to enhance the effectiveness of postural drainage.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
When updating protocols for the use of belt restraints, the nurse manager should include the following guideline:
A) Document the client’s condition every 15 min
Frequent documentation of the client's condition and the need for restraint is essential to monitor their well-being and ensure that restraints are used only when necessary. The other options are not recommended:
B) Requesting a PRN restraint prescription for clients who are aggressive is not appropriate because restraints should only be used when there is an immediate risk to the patient or others, and obtaining a PRN prescription for restraints is generally not standard practice.
C) Attaching the restraint to the bed's side rails is not recommended because restraints should be used as a last resort, and there are specific guidelines for restraint application to ensure patient safety.
D) Removing the client's restraint every is not appropriate either. Restraints should only be removed when the client's condition improves, and alternatives to restraint have been explored, or when it's deemed necessary for the patient's safety and well-being following established protocols and guidelines. The option seems incomplete and does not specify the appropriate time frame for removal.
Correct Answer is B
Explanation
Choice A reason
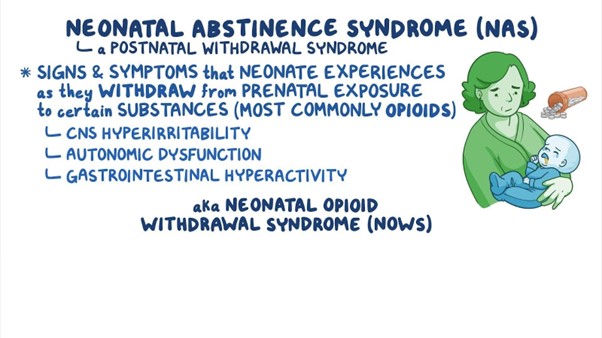
Administering naloxone to the newborn is not appropriate. Naloxone is an opioid antagonist used to reverse the effects of opioid overdose in adults. It is not typically used for newborns with neonatal abstinence syndrome. The management of NAS is primarily supportive, and medications may be prescribed to help manage specific withdrawal symptoms, but naloxone is not a standard treatment for NAS.
Choice B reason:
Minimizing noise in the newborn's environment is a crucial action in the plan of care is the correct action to be included. Newborns experiencing NAS can be easily overstimulated, and loud noises can exacerbate their withdrawal symptoms and distress. Creating a calm and quiet environment helps reduce agitation and promotes better sleep and overall comfort.
Choice C reason
Swaddling the newborn with his leg extended is not appropriate in this case. Swaddling can be beneficial for some newborns, but the specific positioning and swaddling techniques should be individualized based on the newborn's needs and preferences. Extending the newborn's legs may not necessarily be the best approach, as it may not provide comfort or address the symptoms associated with NAS.
Choice D reason:
Maintaining eye contact with the newborn during feedings is not appropriate in this case. While maintaining eye contact during feedings is an essential aspect of bonding and promoting parent-newborn attachment, it may not be the primary focus in managing neonatal abstinence syndrome. The plan of care for a newborn with NAS would primarily involve managing withdrawal symptoms, providing comfort measures, and addressing the newborn's unique needs during this challenging period.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
