A nurse is caring for a newborn whose mother was taking methadone during her pregnancy.
Which of the following findings indicates the newborn is experiencing withdrawal?
Acrocyanosis
Bradycardia
Bulging fontanels
Hypertonicity
The Correct Answer is D
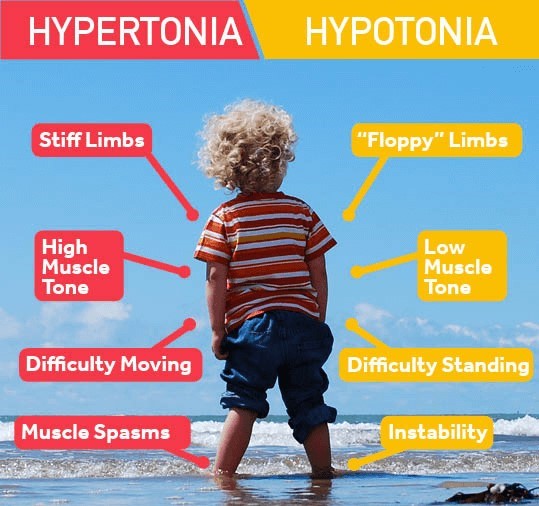
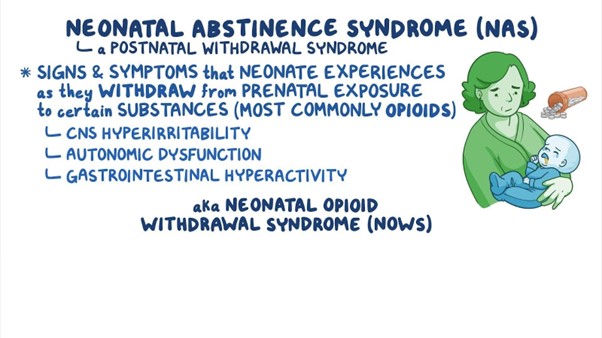
Hypertonicity is a sign of increased muscle tone and stiffness, which can indicate that the newborn is experiencing withdrawal from methadone exposure in utero. Methadone is an opioid medication that can cross the placenta and cause neonatal abstinence syndrome (NAS) in the newborn.
Choice A, acrocyanosis, is wrong because it is a normal finding in newborns.
Acrocyanosis is a bluish discoloration of the hands and feet due to immature peripheral circulation. It usually resolves within the first 24 to 48 hours of life.
Choice B, bradycardia, is wrong because it is not a typical sign of withdrawal.
Bradycardia is a slow heart rate, usually less than 100 beats per minute in newborns. It can be caused by hypoxia, hypothermia, hypoglycemia, or vagal stimulation.
Choice C, bulging fontanels, is wrong because it is a sign of increased intracranial pressure, not withdrawal. Bulging fontanels can be caused by meningitis, hydrocephalus, or hemorrhage.
Normal ranges for newborn vital signs are as follows:
- Heart rate: 120 to 160 beats per minute
- Respiratory rate: 30 to 60 breaths per minute
- Temperature: 36.5 to 37.5°C (97.7 to 99.5°F)
- Blood pressure: 60 to 80 mm Hg systolic and 40 to 50 mm Hg diastolic
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
, dizziness.
Dizziness is a manifestation of hypovolemia, which is a decrease in blood volume due to fluid loss.
Hypovolemia can cause orthostatic hypotension, which is a drop in blood pressure when changing positions. This can lead to dizziness, lightheadedness, or fainting.
Choice A, epistaxis, is wrong because it is not a sign of hypovolemia, but rather a possible cause of it. Epistaxis is a nosebleed that can result from trauma, infection, dryness, or coagulation disorders.
Choice B, headache, is wrong because it is not a specific sign of hypovolemia, but rather a nonspecific symptom that can have many causes. Headache can be associated with dehydration, but it can also be caused by stress, infection, inflammation, or other factors.
Choice D, shortness of breath, is wrong because it is not a sign of hypovolemia, but rather a sign of fluid volume excess.
Fluid volume excess is an increase in blood volume due to fluid retention or overload. Fluid volume excess can cause dyspnea, which is difficulty breathing or shortness of breath.
Normal ranges for blood pressure are 90/60 mm Hg to 120/80 mm Hg for adults.
Normal ranges for heart rate are 60 to 100 beats per minute for adults.
Correct Answer is B
Explanation
Choice A reason
Administering naloxone to the newborn is not appropriate. Naloxone is an opioid antagonist used to reverse the effects of opioid overdose in adults. It is not typically used for newborns with neonatal abstinence syndrome. The management of NAS is primarily supportive, and medications may be prescribed to help manage specific withdrawal symptoms, but naloxone is not a standard treatment for NAS.
Choice B reason:
Minimizing noise in the newborn's environment is a crucial action in the plan of care is the correct action to be included. Newborns experiencing NAS can be easily overstimulated, and loud noises can exacerbate their withdrawal symptoms and distress. Creating a calm and quiet environment helps reduce agitation and promotes better sleep and overall comfort.
Choice C reason
Swaddling the newborn with his leg extended is not appropriate in this case. Swaddling can be beneficial for some newborns, but the specific positioning and swaddling techniques should be individualized based on the newborn's needs and preferences. Extending the newborn's legs may not necessarily be the best approach, as it may not provide comfort or address the symptoms associated with NAS.
Choice D reason:
Maintaining eye contact with the newborn during feedings is not appropriate in this case. While maintaining eye contact during feedings is an essential aspect of bonding and promoting parent-newborn attachment, it may not be the primary focus in managing neonatal abstinence syndrome. The plan of care for a newborn with NAS would primarily involve managing withdrawal symptoms, providing comfort measures, and addressing the newborn's unique needs during this challenging period.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
