A nurse is caring for a client who has an intracranial pressure (ICP) reading of 40 mm Hg. Which of the following findings should the nurse identify as a late sign of ICP? (Select all that apply.)
Slurred speech.
Bradycardia with a bounding pulse.
Confusion.
Hypertension with an increasing pulse pressure.
Nonreactive dilated pupils.
Hypotension with a decreasing pulse pressure.
Correct Answer : B,D,E
The correct answers are b, d, and e.
Choice A: Slurred speech.
Slurred speech can be associated with increased ICP due to the pressure effects on the brain areas responsible for speech production. However, it is not typically considered a late sign of increased ICP. It may occur earlier in the progression as the brain's ability to coordinate muscle movements is affected.
Choice B: Bradycardia with a bounding pulse.
Bradycardia with a bounding pulse is a classic sign of Cushing's triad, which is a late and ominous sign of significantly increased ICP. It indicates that the body is attempting to increase arterial blood pressure to overcome the increased ICP and maintain cerebral perfusion. The normal range for adult heart rate is 60-100 beats per minute.
Choice C: Confusion.
Confusion can be an early sign of increased ICP as it can indicate changes in cerebral function. However, it is not specifically a late sign of increased ICP. Early signs of increased ICP can include headache, nausea, and confusion, as the brain is initially responding to the pressure changes.
Choice D: Hypertension with an increasing pulse pressure.
Hypertension with an increasing pulse pressure is another component of Cushing's triad. It reflects the body's compensatory mechanism to preserve cerebral blood flow in the face of rising ICP. An increasing pulse pressure (the difference between systolic and diastolic blood pressure) is a late sign of increased ICP. Normal pulse pressure is typically 30-40 mm Hg.
Choice E: Nonreactive dilated pupils.
Nonreactive dilated pupils are a late sign of increased ICP and indicate pressure on the cranial nerves that control pupil size and reaction to light. This is a grave sign and often indicates impending brain herniation.
Choice F: Hypotension with a decreasing pulse pressure.
Hypotension with a decreasing pulse pressure is not typically associated with increased ICP. In fact, hypertension with a widening pulse pressure would be more indicative of increased ICP as part of Cushing's triad.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
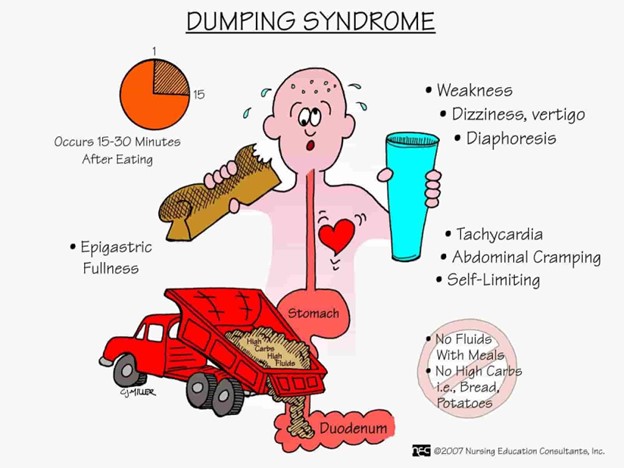
Choice A Reason: Sweating and pallor are early signs and symptoms of dumping syndrome, which is a condition where food moves too quickly from the stomach to the small intestine, causing rapid fluid shifts and hormonal changes. Sweating and pallor are caused by hypoglycemia, which occurs when the high concentration of food in the small intestine stimulates insulin secretion.
Choice B Reason: Abdominal cramping and pain are late signs and symptoms of dumping syndrome, which occur about one to three hours after eating. Abdominal cramping and pain are caused by intestinal distension, spasms, and gas formation.
Choice C Reason: Double vision and chest pain are not signs and symptoms of dumping syndrome, but may indicate other serious conditions, such as stroke or heart attack. Double vision and chest pain should be reported to the provider immediately.
Choice D Reason: Bradycardia and indigestion are not signs and symptoms of dumping syndrome, but may be related to other gastrointestinal disorders, such as gastritis or peptic ulcer disease. Bradycardia and indigestion should be evaluated by the provider for further diagnosis and treatment.
Correct Answer is D
Explanation
Choice A reason: This is incorrect because applying the medication when you are experiencing eye pain can be ineffective or harmful for treating open-angle glaucoma. Open-angle glaucoma is a chronic condition that causes increased pressure inside the eye and damage to the optic nerve, which can lead to vision loss. Eye pain is not a common symptom of open-angle glaucoma, but rather an indication of acute angle closure glaucoma, which is a medical emergency that requires immediate treatment. The nurse should instruct the client to apply the medication as prescribed, regardless of pain level, and seek medical attention if they experience severe eye pain, headache, nausea, or blurred vision.
Choice B reason: This is incorrect because using the medication only until the intraocular pressure returns to normal can cause recurrence or worsening of open-angle glaucoma. Intraocular pressure is the pressure inside
the eye that can affect eye health and vision. Normal intraocular pressure ranges from 10 to 21 mmHg, but it can vary depending on age, time of day, or other factors. The nurse should instruct the client to monitor their intraocular pressure regularly and report any changes to their provider, but not to stop using
the medication without consulting their provider first.
Choice C reason: This is incorrect because using the medication for approximately 10 days, then gradually tapering off can cause rebound or adverse effects of open-angle glaucoma. The medication for open-angle glaucoma can be either beta-blockers, such as timolol, or cholinergic agents, such as pilocarpine, which work by reducing fluid production or increasing fluid drainage in the eye. The nurse should instruct the client to follow their provider's instructions on how long and how much to use the medication and not to change or discontinue it abruptly without their provider's approval.
Choice D reason: This is correct because applying the medication on a regular schedule for the rest of your life can help control and prevent the progression of open-angle glaucoma. Open-angle glaucoma is a lifelong condition that requires consistent and continuous treatment to maintain normal intraocular pressure and prevent vision loss. The nurse should instruct the client to apply the medication at the same time every day and not to miss or skip any doses. The nurse should also teach the client how to store, handle, and administer the medication properly and safely.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
