A nurse is caring for a client who has anorexia nervosa and a behavioral management plan in place. Which of the following findings should the nurse identify as an indication that the behavioral plan is effective?
Potassium 3.5 mEq/L
Sodium 130 mEq/L
Hgb 10 g/dL
BMI 14.5
The Correct Answer is A
The normal range for potassium levels is generally between 3.5 to 5.0 mEq/L. A potassium level of 3.5 mEq/L falls within the lower end of the normal range, suggesting that the client's potassium levels are relatively stable. This finding alone does not indicate the overall effectiveness of the behavioral plan.
The normal range for sodium levels is typically between 135 to 145 mEq/L. A sodium level of 130 mEq/L falls below the normal range and indicates hyponatremia (low sodium levels). Hyponatremia can be a cause for concern, and it suggests that the behavioral management plan may need further attention or adjustments.
The normal range for hemoglobin (Hgb) levels varies depending on factors such as age and gender. However, in general, a Hgb level of 10 g/dL falls below the normal range and indicates anemia. Anemia is a common complication in individuals with anorexia nervosa and can result from inadequate nutrient intake. This finding suggests that the behavioral plan may need further evaluation and adjustment to address the client's nutritional needs.
Body Mass Index (BMI) is a measure that relates weight and height. A BMI of 14.5 indicates severe underweight and is well below the normal range. This finding suggests that the client's nutritional status is still significantly compromised, and the behavioral management plan may require further attention to support weight restoration and overall recovery.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
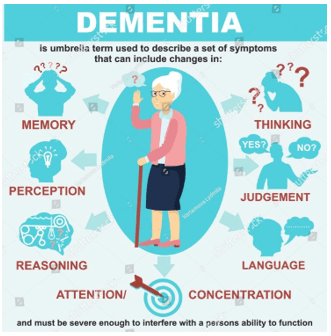
a. Memory loss that disrupts ADLs
Explanation: Dementia is a condition characterized by a decline in cognitive function that affects a person's ability to perform activities of daily living (ADLs). Memory loss is a common symptom of dementia, particularly in the early stages. The memory loss can disrupt a person's ability to carry out tasks they were previously able to do independently, such as dressing, bathing, and eating. Therefore, option a is the correct answer.
Option b, catatonia, is a condition characterized by a lack of movement or activity, which is not typically associated with dementia.
Option c, illusions, involve a misinterpretation of sensory information and may occur in some forms of dementia but are not a defining feature.
Option d, pressured speech, is a symptom commonly associated with mania or bipolar disorder, but is not typically seen in dementia.
Correct Answer is A
Explanation
Whenever a medication error occurs, it should be documented in an incident report. The purpose of the incident report is to document the details of the event, including what happened, why it happened, and what was done to prevent it from happening again. Incident reports are not part of the client's medical record and are not used for disciplinary action. They are used for quality improvement and risk management purposes.
The nursing care plan is a document that outlines the client's nursing care needs and interventions. It is not the appropriate place to document a medication error.
The controlled substance inventory record is used to document the administration and dispensing of controlled substances. It is not the appropriate place to document a medication error.
The provider's progress notes document the provider's assessment, diagnosis, and treatment plan for the client. They are not the appropriate place to document a medication error.

Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
