A nurse is caring for a toddler who has acute laryngotracheobronchitis and has been placed in a cool mist tent. Which of the following findings indicates that the treatment has been effective?
Barking cough
Decreased stridor
Improved hydration
Decreased temperature
The Correct Answer is B
Choice A: A barking cough is not a finding that indicates that the treatment has been effective, but rather a symptom of acute laryngotracheobronchitis, which is also known as croup. Croup is a condition that causes inflammation and narrowing of the upper airway and produces a characteristic barking or seal-like cough. A barking cough may persist for several days after the onset of croup and does not reflect the severity of the airway obstruction.
Choice B: Decreased stridor is a finding that indicates that the treatment has been effective, as stridor is a sign of airway obstruction caused by acute laryngotracheobronchitis. Stridor is a high-pitched, noisy breathing sound that occurs when the air passes through the narrowed airway. Stridor may be inspiratory, expiratory, or biphasic,
depending on the level of obstruction. Decreased stridor means that the airway is less obstructed and the child can breathe more easily.
Choice C: Improved hydration is not a finding that indicates that the treatment has been effective, but rather a goal of treatment for acute laryngotracheobronchitis. Dehydration can worsen the symptoms and complications of croup by thickening the mucus and increasing the risk of infection. Improved hydration can help thin out the mucus and prevent dehydration. Hydration can be improved by encouraging oral fluids, administering intravenous fluids, or providing humidified air.
Choice D: Decreased temperature is not a finding that indicates that the treatment has been effective, but rather a possible outcome of treatment for acute laryngotracheobronchitis. Fever may or may not be present in croup, depending on the cause and severity of the condition. Fever can be caused by viral or bacterial infection, inflammation, or dehydration. Decreased temperature can indicate that the infection or inflammation is resolving or that the dehydration is corrected.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Choice A: This test will not indicate if the child has rheumatic fever, as rheumatic fever is a complication of an untreated or inadequately treated streptococcal infection that affects the heart, joints, skin, and brain. Rheumatic fever is diagnosed based on clinical criteria, such as carditis, polyarthritis, chorea, erythema marginatum, and subcutaneous nodules.
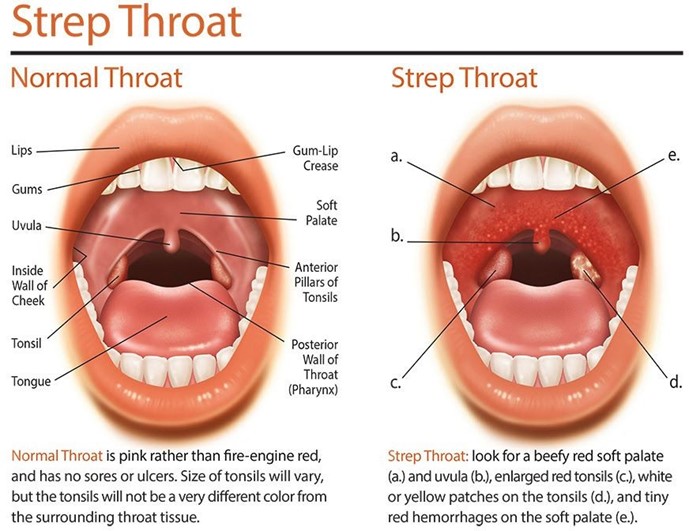
Choice B: This test will confirm if the child had a recent streptococcal infection, as antistreptolysin O (ASO) is an antibody that the body produces in response to streptococcal bacteria. A high ASO titer indicates that the child was exposed to streptococcal bacteria within the past few weeks. A streptococcal infection can cause pharyngitis, tonsillitis, scarlet fever, or impetigo.
Choice C: This test will not indicate if the child has a therapeutic blood level of an aminoglycoside, as an aminoglycoside is a type of antibiotic that is used to treat serious bacterial infections. A therapeutic blood level of an aminoglycoside means that the drug is effective and safe in the body. A therapeutic blood level of an aminoglycoside is measured by a peak and trough level.
Choice D: This test will not confirm if the child has immunity to streptococcal bacteria, as immunity to streptococcal bacteria means that the body can resist or fight the infection. Immunity to streptococcal bacteria can be acquired by natural exposure or vaccination. Immunity to streptococcal bacteria is measured by an antibody titer or a skin test.
Correct Answer is A
Explanation
Choice A reason: This is a therapeutic response that acknowledges the parent's feelings and provides reassurance that the behavior is normal and temporary. The other responses are either dismissive, judgmental, or self-disclosing, which are not helpful for the parent.
Choice B reason: This is a judgmental response that implies that the parent is overreacting or has unrealistic expectations for their child.
Choice C reason: This is a dismissive response that minimizes the parent's concern and does not offer any support
or information.
Choice D reason: This is a self-disclosing response that shifts the focus from the parent to the nurse and does not
address the issue at hand.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
