A nurse is collecting data from a client who is 14 hr postpartum. The nurse notes breasts soft, fundus firm, slightly deviated to the right; moderate lochia rubra; temperature 37.7° C (100° F), pulse rate 88/min, respiratory rate 18/min. Which of the following actions should the nurse perform?
Encourage the client to nurse more frequently so her milk will come in.
Increase IV fluids.
Ask the client to empty her bladder.
Report the client's temperature elevation.
The Correct Answer is C
Choice A reason: Encourage the client to nurse more frequently so her milk will come in is incorrect, as this action is not related to the data collected by the nurse. The nurse notes that the client's breasts are soft, which indicates that the milk has not come in yet. This is normal and expected for a client who is 14 hr postpartum, as milk production usually begins around 72 to 96 hr after birth. The nurse should encourage the client to nurse frequently and effectively to stimulate milk production and prevent engorgement.
Choice B reason: Increase IV fluids is incorrect, as this action is not indicated by the data collected by the nurse. The nurse notes that the client's vital signs are within normal limits, except for a slight temperature elevation. Increasing IV fluids can cause fluid overload and electrolyte imbalance in the client. The nurse should maintain the IV fluids at the prescribed rate and monitor the client's intake and output.
Choice C reason: Ask the client to empty her bladder is correct, as this action is indicated by the data collected by the nurse. The nurse notes that the client's fundus is firm but slightly deviated to the right, which suggests bladder distension. A full bladder can interfere with uterine contraction and involution and increase the risk of hemorrhage and infection. The nurse should assist the client to empty their bladder and reassess the fundal position.
Choice D reason: Report the client's temperature elevation is incorrect, as this action is not necessary for a slight temperature elevation in a postpartum client. The nurse notes that the client's temperature is 37.7° C (100° F), which is slightly above normal but within the range of expected findings for a postpartum client. A mild temperature elevation in the first 24 hr after birth can be due to dehydration, exertion, or hormonal changes and does not indicate infection. The nurse should encourage oral fluid intake and monitor the temperature every 4 hr.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
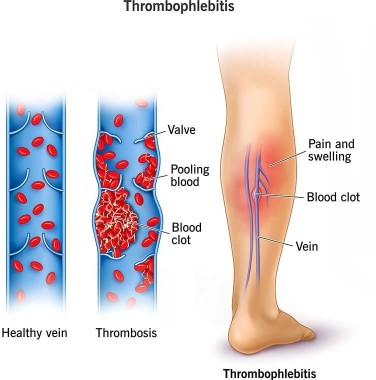
Choice A reason: Apply warm, moist soaks to the client's lower legs is incorrect, as this action is not effective for preventing thrombophlebitis. Warm, moist soaks can provide comfort and reduce inflammation, but they do not improve blood circulation or prevent clot formation.
Choice B reason: Have the client ambulate frequently in the hallway is correct, as this action can prevent thrombophlebitis by improving venous return and preventing stasis. The nurse should encourage and assist the client to ambulate early and frequently after a cesarean birth, as long as there are no contraindications. The nurse should also monitor the client for signs of orthostatic hypotension and provide support as needed.
Choice C reason: Keep the client on bed rest is incorrect, as this action can increase the risk of thrombophlebitis by reducing blood flow and promoting stasis. Bed rest can also delay wound healing and increase the risk of infection and deconditioning. The nurse should avoid keeping the client on bed rest unless absolutely necessary.
Choice D reason: Place pillows under the client's knees while she is resting in bed is incorrect, as this action can impair blood circulation and increase the risk of thrombophlebitis. Placing pillows under the knees can cause pressure on the popliteal veins and reduce venous return. The nurse should advise the client to avoid crossing their legs or placing pillows under their knees while resting in bed.
Correct Answer is D
Explanation
Choice A reason: "Babies know instinctively exactly how much of the nipple to take into their mouth." is incorrect, as this response does not provide adequate guidance or support for the client. Babies may not always latch on correctly or effectively, especially in the first few atempts. The nurse should teach the client how to position and latch the baby properly and observe for signs of effective breastfeeding.
Choice B reason: "Your baby's mouth is rather small so she will only take part of the nipple." is incorrect, as this response can lead to ineffective breastfeeding and nipple trauma. Taking only part of the nipple can cause poor milk transfer, inadequate milk production, and nipple soreness or cracking. The nurse should teach the client how to ensure that the baby takes enough of the nipple and areola into their mouth.
Choice C reason: "Try to place the nipple, the entire areola, and some breast tissue beyond the areola into her mouth." -Including too much breast tissue can be uncomfortable. While some areola is important, including too much breast tissue can hinder proper latch and milk flow.
Choice D reason: "You should place your nipple and some of the areola into her mouth." This accurately describes the ideal latch for breastfeeding. Including some of the areola helps the baby latch deeply and comfortably, promoting milk transfer and preventing feeding difficulties and nipple soreness.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
