A nurse is collecting data from an infant a large patent ductus arteriosus. Which of the following is clinical manifestations should the nurse expect?
Machine like murmur
Chronic hypoxemia
Cyanosis with crying
Weak pulse
The Correct Answer is A
A. Machine-like murmur.
This option is correct. A characteristic clinical manifestation of a large patent ductus arteriosus is a continuous "machine-like" murmur heard on auscultation. This murmur is typically heard best at the upper left sternal border and may radiate to the back.
B. Chronic hypoxemia.
Chronic hypoxemia is not typically a primary manifestation of a large PDA. While PDA can lead to increased pulmonary blood flow and potentially contribute to pulmonary congestion, chronic hypoxemia may not be a prominent feature unless complications such as heart failure develop.
C. Cyanosis with crying.
Cyanosis with crying is more commonly associated with cyanotic congenital heart defects such as tetralogy of Fallot. While PDA can contribute to cyanosis in certain circumstances, it is not typically a consistent clinical manifestation.
D. Weak pulse.
A weak pulse is not typically associated specifically with a large PDA. Infants with PDA may have bounding pulses due to increased blood flow through the ductus arteriosus.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
A. "I will elevate the affected area if possible."
This statement is correct. Elevating the affected area can help reduce swelling and minimize bleeding by promoting venous return. Elevating the limb above the level of the heart can aid in controlling bleeding and is a recommended intervention.
B. "I will apply warm compresses over the site."
This statement is incorrect. Applying warm compresses is generally not recommended for controlling bleeding in hemophilia. Heat can increase blood flow to the area, potentially exacerbating bleeding. Cold compresses or ice packs are typically recommended to help constrict blood vessels and reduce bleeding.
C. "I will have my child rest."
This statement is correct. Resting is an essential component of managing bleeding episodes in children with hemophilia. Physical activity and exertion can increase the risk of injury and bleeding, so it's important for children with hemophilia to avoid strenuous activities during bleeding episodes.
D. "I will promptly mobilize the involved area to relieve pain & decrease bleeding."
Immobilizing the affected area can help control bleeding and reduce pain by minimizing movement. This is also an appropriate response.
Correct Answer is D
Explanation
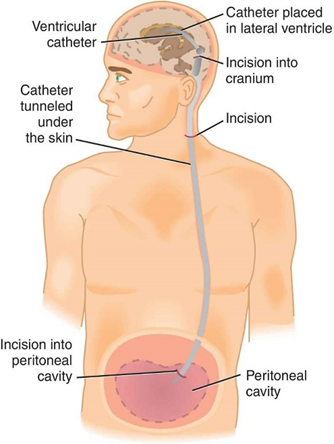
A. A 45-degree head elevation: This position can help facilitate venous drainage and reduce intracranial pressure. Elevating the head of the bed may aid in preventing the accumulation of cerebrospinal fluid (CSF) in the brain, which is important after VP shunt insertion to maintain proper drainage. However, this position alone may not be sufficient.
B. On the nonoperative side: Placing the child on the nonoperative side can help reduce pressure on the side where the shunt was inserted, minimizing discomfort and the risk of disruption or displacement of the shunt. However, this position may not directly affect CSF drainage.
C. Prone: Placing the child prone (lying face down) is generally not recommended after VP shunt insertion. This position may increase pressure on the head and interfere with proper CSF drainage, potentially leading to complications.
D. Supine: Placing the child supine (lying on their back) is typically recommended after VP shunt insertion. This position helps promote proper drainage of CSF through the shunt system without placing undue pressure on the surgical site. It also allows for easy monitoring of the child's condition and surgical site.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
