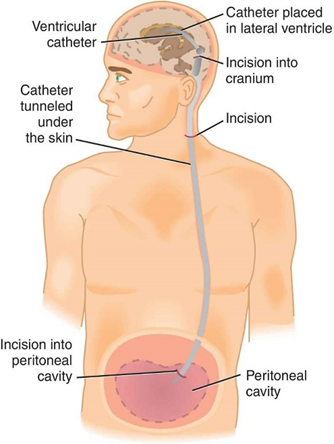
A nurse is caring for a child who is postoperative following the insertion of a ventriculoperitoneal shunt. The nurse should place the child in which of the following positions?
A 45 degree head elevation
On the nonoperative side
Prone
Supine
The Correct Answer is D
A. A 45-degree head elevation: This position can help facilitate venous drainage and reduce intracranial pressure. Elevating the head of the bed may aid in preventing the accumulation of cerebrospinal fluid (CSF) in the brain, which is important after VP shunt insertion to maintain proper drainage. However, this position alone may not be sufficient.
B. On the nonoperative side: Placing the child on the nonoperative side can help reduce pressure on the side where the shunt was inserted, minimizing discomfort and the risk of disruption or displacement of the shunt. However, this position may not directly affect CSF drainage.
C. Prone: Placing the child prone (lying face down) is generally not recommended after VP shunt insertion. This position may increase pressure on the head and interfere with proper CSF drainage, potentially leading to complications.
D. Supine: Placing the child supine (lying on their back) is typically recommended after VP shunt insertion. This position helps promote proper drainage of CSF through the shunt system without placing undue pressure on the surgical site. It also allows for easy monitoring of the child's condition and surgical site.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
A. Drooling:
Drooling can occur post-tonsillectomy due to throat discomfort or swelling. However, it is not specific to hemorrhage. It may result from pain, swelling, or difficulty swallowing.
B. Continuous swallowing:
Continuous swallowing is indeed a clinical manifestation of hemorrhage after a tonsillectomy. The presence of blood in the throat triggers the swallowing reflex, leading to frequent swallowing by the patient. This symptom is characteristic of hemorrhage and requires immediate medical attention.
C. Poor fluid intake:
Poor fluid intake can occur post-tonsillectomy due to pain, discomfort, or nausea. While it can be a concern for overall recovery, it is not specific to hemorrhage.
D. Increased pain:
Increased pain can be associated with hemorrhage, especially if it is sudden, severe, or worsening. However, it is not as specific as continuous swallowing in indicating hemorrhage post-tonsillectomy. Increased pain can also be due to various other reasons such as inflammation, infection, or trauma.
Correct Answer is A
Explanation
A. Lethargy: Lethargy can be a concerning sign in a postoperative child, especially following a procedure involving the central nervous system like VP shunt insertion. It could indicate increased intracranial pressure or other neurological complications, which require immediate attention. Therefore, this is a priority finding.
B. Urine output 70 mL in 2 hr: While monitoring urine output is important for assessing hydration and renal function, a urine output of 70 mL in 2 hours may not be immediately concerning in a 4-year-old child. However, if this pattern continues or if there are signs of dehydration, it should be addressed. It's not as urgent as assessing for neurological changes.
C. Lying flat on the unaffected side: The positioning of the child, lying flat on the unaffected side, may or may not be concerning depending on the specific instructions provided postoperatively. While positioning can affect the function of the VP shunt, it may not necessarily indicate an immediate complication.
D. Respiratory rate 20/min: A respiratory rate of 20 breaths per minute is within the normal range for a 4-year-old child. While changes in respiratory rate can indicate respiratory distress, this respiratory rate alone is not immediately concerning.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
