A nurse is collecting data from an infant who has coarctation of the aorta. Which of the following manifestations should the nurse expect?
Machine-like murmur
Severe cyanosis
Decreased blood pressure in the legs
Pulmonary edema
The Correct Answer is C
A. Machine-like murmur:
A machine-like murmur typically refers to a continuous murmur, which can be heard throughout systole and diastole. While machine-like murmurs can be associated with certain cardiac conditions, such as patent ductus arteriosus (PDA), they are not typically heard in coarctation of the aorta. In coarctation of the aorta, a systolic ejection murmur may be heard over the upper left sternal border due to turbulent blood flow across the narrowed aortic segment.
B. Severe cyanosis:
Cyanosis refers to a bluish discoloration of the skin and mucous membranes due to decreased oxygenation of the blood. While cyanosis can occur in various congenital heart defects, such as tetralogy of Fallot, it is not a characteristic manifestation of coarctation of the aorta. Coarctation of the aorta typically results in decreased blood flow to the lower extremities rather than mixing of oxygenated and deoxygenated blood.
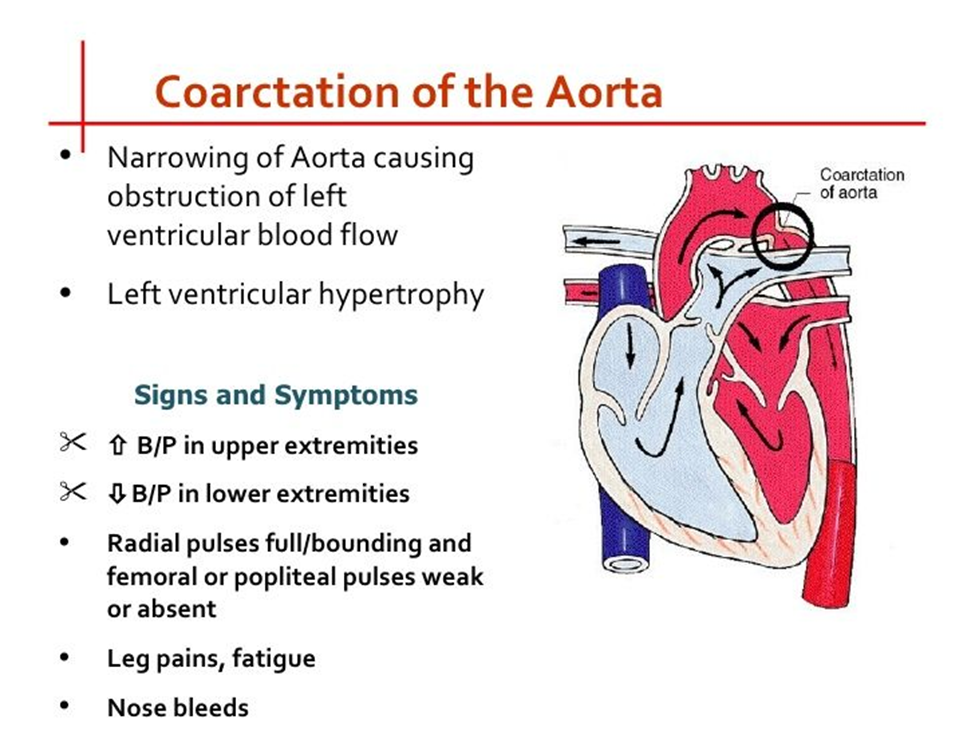
C. Decreased blood pressure in the legs:
This is the correct choice. Coarctation of the aorta is characterized by narrowing of the aorta, which leads to decreased blood flow to the lower extremities. Consequently, blood pressure measurements in the legs may be lower compared to those in the arms. This finding is often a key indicator of coarctation of the aorta.
D. Pulmonary edema:
Pulmonary edema refers to the accumulation of fluid in the lungs and is typically associated with conditions such as heart failure or fluid overload. While some congenital heart defects may lead to heart failure and subsequent pulmonary edema, coarctation of the aorta does not directly cause pulmonary edema. Instead, it primarily affects blood flow to the lower extremities due to the narrowing of the aorta.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
A. Onlooker play:
Onlooker play is when a child observes others playing without actively participating themselves. This type of play typically involves watching others engage in activities or play without joining in. It does not directly involve role-playing or hands-on activities to prepare a child for surgery.
B. Therapeutic play:
This is the correct answer. Therapeutic play involves using play activities to help children express their feelings, fears, and concerns about medical procedures or hospitalization. It often includes role-playing and hands-on activities such as practicing medical procedures on dolls or stuffed animals. Therapeutic play helps children become familiar with medical equipment and procedures in a non-threatening environment, reducing anxiety and promoting coping skills.
C. Cooperative play:
Cooperative play involves children playing together, interacting, and collaborating in shared activities. While cooperative play can be beneficial for social development, it does not necessarily involve role-playing or hands-on activities specific to preparing a child for surgery.
D. Play therapy:
Play therapy is a form of psychotherapy that uses play to communicate with and help children express their thoughts and emotions. While play therapy can be therapeutic for children dealing with various issues, including medical procedures, it is typically facilitated by a trained therapist rather than being directly utilized to prepare a child for surgery through role-playing or hands-on activities.
Correct Answer is A
Explanation
A. Upright: This position allows for better expansion of the lungs and improved ventilation-perfusion matching, as gravity helps the diaphragm move downward and expand the lungs. It is often beneficial for patients with respiratory distress or failure.
B. Supine: While lying flat on the back (supine position) may be comfortable for some patients, it can restrict lung expansion, especially in individuals with compromised respiratory function. This position may not be ideal for maximal lung expansion in this scenario.
C. Prone: The prone position involves lying flat on the abdomen. In some cases, especially in adults with acute respiratory distress syndrome (ARDS), prone positioning has been shown to improve oxygenation by optimizing lung mechanics. However, it may not be practical or comfortable for all patients and is not typically used as a first-line intervention in school-age children with pneumonia.
D. Side-lying: While side-lying positions can sometimes improve lung expansion on the dependent side, it may not be as effective as the upright position in maximizing lung expansion, especially in cases of respiratory failure.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
