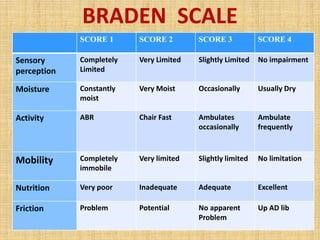
A nurse is completing a risk assessment on a new admission. Which standardized scale will the nurse use to calculate the client's risk for pressure ulcers?
Morse Scale
Braden Scale
Bristol Scale
Hendrich II scale
The Correct Answer is B
A. Morse Scale:
The Morse Scale, also known as the Morse Fall Scale, is used to assess a patient's risk of falling. It evaluates various factors such as history of falling, secondary diagnosis, ambulatory aids, IV therapy, gait, and mental status. It is primarily focused on assessing the risk of falls, not pressure ulcers.
B. Braden Scale:
As previously mentioned, the Braden Scale assesses a patient's risk for developing pressure ulcers. It takes into account sensory perception, moisture, activity, mobility, nutrition, and friction/shear. The scale helps healthcare providers determine the level of risk a patient has for developing pressure sores and guides interventions to prevent them.
C. Bristol Scale:
The Bristol Stool Scale is used to classify the form of human feces into seven categories. It is a medical aid designed to classify the form of human feces into seven categories. This scale is primarily used to assess bowel movements and is unrelated to pressure ulcers.
D. Hendrich II Scale:
The Hendrich II Fall Risk Model is a tool designed to identify patients at risk for falls. It includes factors such as confusion, symptomatic depression, altered elimination, dizziness, male gender, and the use of antiepileptics, benzodiazepines, or non-opioid analgesics. Similar to the Morse Scale, it focuses on assessing the risk of falls, not pressure ulcers.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
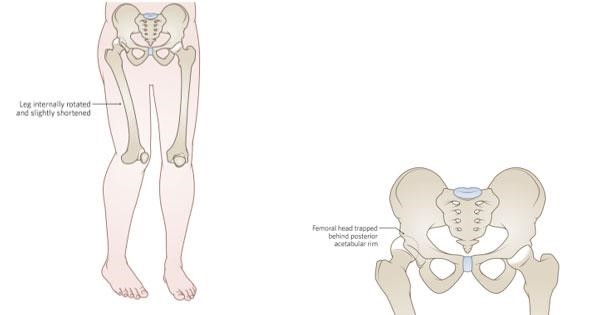
Correct Answer is A
Explanation
A. Right hip dislocation: In a hip dislocation, the head of the femur is forced out of the acetabulum, which is the socket in the pelvis. This can cause a noticeably shorter leg, hip deformity, and acute pain. Imaging might not show a fracture in the case of a dislocation.
B. Right hip contusion: A hip contusion is a bruise on the hip, usually caused by a direct blow or trauma. While it can cause pain and swelling, it typically does not result in a noticeably shorter leg or hip deformity.
C. Right hip strain: Hip strain refers to damage to the muscles or tendons around the hip joint due to overuse or sudden twisting movements. While it can cause pain, it does not typically lead to a noticeable leg shortening or hip deformity.
D. Right hip osteoarthritis: Osteoarthritis is a degenerative joint disease that can affect the hip joint. It leads to joint pain and stiffness but does not usually cause a noticeable leg shortening or acute deformity unless there are severe complications, which are not mentioned in the scenario.
Correct Answer is A
Explanation
A. Apply a moisture barrier ointment to the client's skin
Applying a moisture barrier ointment creates a protective barrier on the skin, preventing prolonged exposure to moisture, which can lead to skin breakdown in individuals with urinary incontinence. Keeping the skin dry and protected is essential in preventing skin irritation and breakdown.
B. Check the client's skin every 8 hr for signs of breakdown - Skin should be assessed more frequently, ideally every 2-4 hours, especially in clients with urinary incontinence, to detect signs of breakdown early.
C. Clean the client's skin and perineum with hot water after each episode of incontinence - Hot water can be harsh on the skin and exacerbate irritation. It's recommended to use mild, warm water and gentle cleansing techniques. Harsh cleaning methods can damage the skin.
D. Request a prescription for the insertion of an indwelling urinary catheter - Indwelling urinary catheters pose an increased risk of infection and other complications. Catheters should only be used when absolutely necessary, and preventive measures should be taken to manage incontinence without catheterization whenever possible.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
