A nurse is contributing to the plan of care for a client who is starting bowel training for the management of fecal incontinence. Which of the following interventions should the nurse recommend?
Assist the client to the restroom 30 min after meals.
Limit the client's physical activity until bowel continence is achieved.
Limit the client's fluid intake to 1500 mL/day.
Instruct the client to limit their intake of high-fiber foods
The Correct Answer is A
Choice A Reason:
Assisting the client to the restroom 30 minutes after meals is correct recommendation. This intervention aligns with the natural response of the gastrocolic reflex, which often leads to increased colonic motility after eating. Timing the restroom visit to this period can take advantage of the body's natural tendency to have a bowel movement after meals, potentially aiding in achieving bowel continence.
Choice B Reason:
Limiting the client's physical activity until bowel continence is achieved is not appropriate. Physical activity can actually stimulate bowel function and regularity. Moderate physical activity, as appropriate for the client's condition, can promote regular bowel movements. Restricting physical activity might hinder the overall success of bowel training.
Choice C Reason:
Limiting the client's fluid intake to 1500 mL/day is not appropriate. Adequate hydration is crucial for bowel health and regularity. Limiting fluid intake could lead to dehydration and constipation, which can exacerbate fecal incontinence. It's important to encourage adequate hydration unless there are specific medical reasons to restrict fluids.
Choice D Reason:
Instructing the client to limit their intake of high-fiber foods is incorrect. High-fiber foods are beneficial for bowel regularity and can help manage fecal incontinence by promoting healthy bowel movements. Limiting high-fiber foods could potentially lead to constipation or exacerbate the issue of fecal incontinence.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Choice A Reason:
Replace the unit when the drainage chamber is full is correct. Regularly emptying the drainage chamber when it becomes full is essential to ensure the drainage system functions properly and continues to effectively remove fluids or air from the chest cavity.
Choice B Reason:
Clamp the tube for 30 min every 8 hr. is incorrect.
Clamping a chest tube without a specific medical order or indication can lead to complications such as a buildup of pressure within the chest cavity or potential damage to the lungs. It's generally not a routine action to clamp the tube without proper instruction.
Choice C Reason:
Pin the tubing to the client's bed sheets is incorrect. Pinning the tubing to the bed sheets can cause tension on the chest tube, leading to accidental dislodgment or obstruction. The tubing should be secured but not pinned to prevent inadvertent movement.
Choice D Reason:
Monitor for at least 150 mL of drainage every hour is incorrect. There isn't a standard or prescribed amount of drainage that should occur hourly. The nurse should monitor the drainage rate and characteristics but shouldn't expect a specific volume within a set timeframe. Monitoring for excessive or decreased drainage and changes in characteristics is crucial, but an hourly volume expectation isn't appropriate.
Correct Answer is A
Explanation
Choice A Reason:
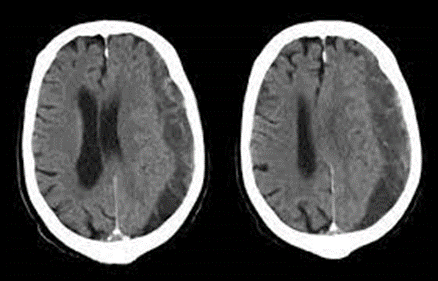
The client has a delayed response to verbal commands. This finding can indicate increased intracranial pressure. Changes in responsiveness, such as delayed responses to verbal commands or other stimuli, can be indicative of neurological impairment due to elevated pressure within the skull.
Choice B Reason:
The client has ecchymosis around the eyes. Ecchymosis around the eyes (raccoon eyes) can occur with certain head injuries, but it's not a direct sign of increased intracranial pressure. It's more commonly associated with basilar skull fractures rather than specifically reflecting increased pressure within the skull.
Choice C Reason:
The client is unable to remember details of the motor-vehicle crash. Memory impairment or amnesia regarding the event can occur due to head trauma, but it might not directly correlate with an increase in intracranial pressure. It's more related to the effects of the injury on memory function.
Choice D Reason:
The client reports ringing in the ears. Tinnitus or ringing in the ears might occur in some cases of head trauma but is not a direct indicator of increased intracranial pressure. It might result from the impact of the injury or other associated factors.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
