A nurse is educating a client with systemic lupus erythematosus about the use of prednisone. Which piece of information should be prioritized?
Prednisone should never be discontinued abruptly.
Long-term effects of prednisone include redistribution of fat.
Prednisone can lead to sodium and fluid retention.
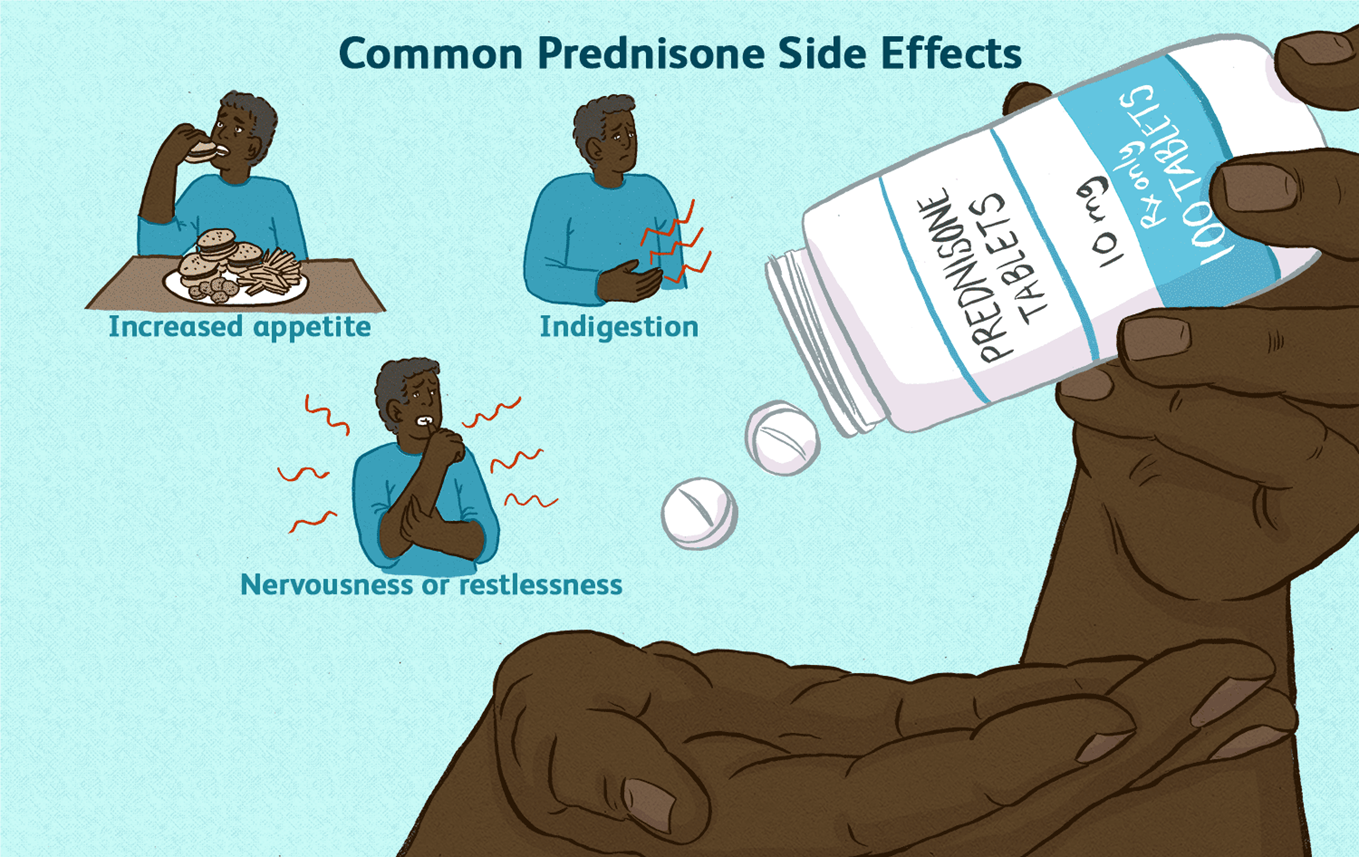
Prednisone might cause the client to feel jittery or nervous.
The Correct Answer is A
Choice A rationale:
Prednisone is a corticosteroid that suppresses the body's natural production of cortisol. Cortisol is a hormone that is essential for life, and it plays a role in many important bodily functions, including:
Regulating blood sugar levels Maintaining blood pressure Reducing inflammation Responding to stress
When a person takes prednisone for a long period of time, their body begins to rely on the medication to provide cortisol. If the medication is stopped suddenly, the body cannot produce enough cortisol on its own, which can lead to a life-threatening condition called adrenal insufficiency.
Adrenal insufficiency can cause a variety of symptoms, including: Extreme fatigue
Weakness Dizziness Nausea Vomiting Abdominal pain Confusion
Loss of consciousness
To prevent adrenal insufficiency, it is important to taper off prednisone slowly over a period of time. This allows the body to gradually adjust to producing cortisol on its own.
Here are some additional details about why prednisone should never be discontinued abruptly: The risk of adrenal insufficiency is highest when prednisone has been taken for more than 3 weeks. The longer a person has been taking prednisone, the slower the taper should be.
It is important to follow the tapering instructions provided by the healthcare provider.
If a person experiences any symptoms of adrenal insufficiency, they should seek medical attention immediately.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Choice A rationale:
It is crucial to prioritize the patient's spouse's emotional needs and preferences during this highly stressful and sensitive situation. Offering the choice to be present during resuscitation demonstrates respect for their autonomy, promotes family- centered care, and facilitates coping mechanisms.
Key considerations supporting this approach:
Respect for Autonomy:
Patients and their loved ones have the right to make informed decisions about their care, including being present during resuscitation efforts.
Respecting this right fosters trust, empowers the spouse, and aligns with ethical principles of patient autonomy. Family-Centered Care:
Family-centered care recognizes the importance of family members in the patient's care and decision-making.
Inviting the spouse to be present demonstrates a commitment to including them in the care process and supporting their emotional needs.
Facilitating Coping Mechanisms:
Witnessing resuscitation efforts can be distressing, but it can also provide closure, acceptance, and the opportunity to say goodbye.
Some individuals find comfort in being present and actively involved, even in difficult circumstances. The nurse can provide emotional support and guidance throughout the process.
Potential Benefits of Presence:
Studies have shown that family presence during resuscitation can have positive outcomes, such as decreased anxiety and post- traumatic stress disorder (PTSD) symptoms in family members.
It may also contribute to greater satisfaction with care and a sense of peace for those who choose to be present.
Rationales for other choices:
Choice B: Requesting that the spouse sit in the waiting room may isolate them and increase their anxiety. It deprives them of the opportunity to be involved in decision-making and potentially delays their grieving process.
Choice C: While the hospital's crisis team can provide valuable support, immediate referral may not align with the spouse's immediate needs or preferences. It's essential to first assess their emotional state and offer the choice of being present.
Choice D: Suggesting prayer may be appropriate for some individuals, but it should not be the first or only option presented. It's important to respect the spouse's spiritual beliefs and offer a range of support options.
Correct Answer is A
Explanation
Choice A rationale:
Assessing the patient's adherence to the drug regimen is the most crucial first step in this situation. Here's a comprehensive explanation:
1. Significance of Adherence in HIV Treatment:
Viral Suppression and Disease Progression: Adherence to antiretroviral therapy (ART) is paramount in HIV management. It directly impacts viral suppression, preventing disease progression, and reducing the risk of opportunistic infections and complications. Non-adherence can lead to viral rebound, increased viral load, and potential disease advancement.
Primary Cause of Treatment Failure: Suboptimal adherence is the leading cause of treatment failure in HIV patients. It can result in:
Reduced effectiveness of ART Development of drug resistance Increased healthcare costs Increased risk of transmission
2. Rationale for Prioritizing Adherence Assessment:
Direct Link to Viral Load and Health Status: A sudden decline in health status and a significant increase in viral load strongly suggest potential non-adherence. Assessing adherence early on can:
Identify the root cause of the clinical deterioration
Inform timely interventions to address adherence barriers Prevent further complications
3. Assessing Adherence Thoroughly:
Non-Judgmental Approach: Creating a supportive and non-judgmental environment is essential for honest and accurate assessment.
Open-Ended Questions: Utilize open-ended questions to explore potential challenges and barriers to adherence, such as: Difficulties with medication schedules
Side effects Financial constraints Forgetfulness
Mental health concerns Substance abuse
Lack of social support
Objective Measures: Complement patient reports with objective measures like:
Pill counts
Pharmacy refill records
Medication Event Monitoring Systems (MEMS)
4. Addressing Adherence Barriers:
Tailored Interventions: Based on the assessment findings, develop individualized strategies to enhance adherence, such as: Simplifying medication regimens
Addressing side effects
Providing medication reminders
Offering counseling and support services
Connecting patients with resources
5. Reassessing and Monitoring:
Continuous Evaluation: Regularly reassess adherence and viral load to ensure treatment effectiveness and make adjustments as needed.
Conclusion:
While other options (B, C, D) may provide valuable information, prioritizing adherence assessment is critical to promptly identify and address potential adherence issues, optimize treatment outcomes, and prevent further health decline in HIV patients experiencing viral rebound.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
