A nurse is evaluating the central venous pressure (CVP) of a client who has sustained multiple traumas. Which of the following interpretations of a low CVP should the nurse make?
Fluid overload
Intracardiac shunt
Hypovolemia
Left ventricular failure
The Correct Answer is C
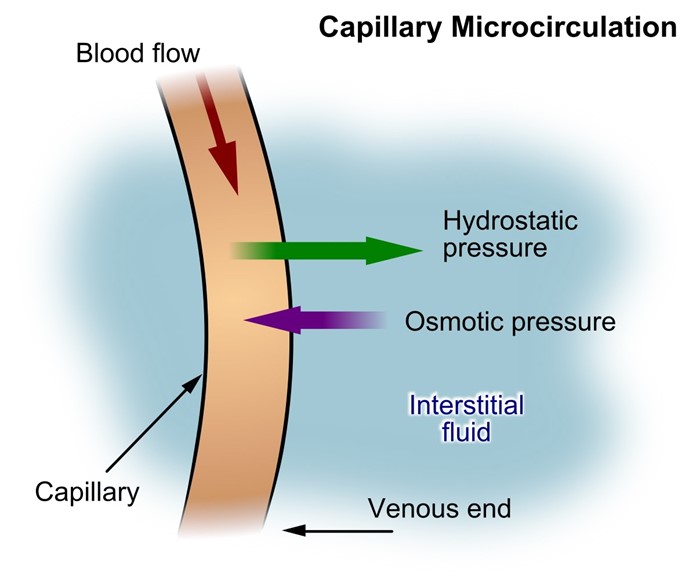
Choice A Reason: This is incorrect because fluid overload is a condition of excess fluid volume in the body. A client who has fluid overload is more likely to have a high CVP, which indicates increased pressure in the right atrium and vena cava.
Choice B Reason: This is incorrect because an intracardiac shunt is a condition of abnormal blood flow between the chambers of the heart. A client who has an intracardiac shunt may have a normal or high CVP, depending on the direction and magnitude of the shunt.
Choice C Reason: This is correct because hypovolemia is a condition of low fluid volume in the body. A client who has hypovolemia is more likely to have a low CVP, which indicates decreased pressure in the right atrium and vena cava.
Choice D Reason: This is incorrect because left ventricular failure is a condition of impaired pumping function of the left ventricle. A client who has left ventricular failure may have a normal or high CVP, depending on the degree of backward failure and pulmonary congestion.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
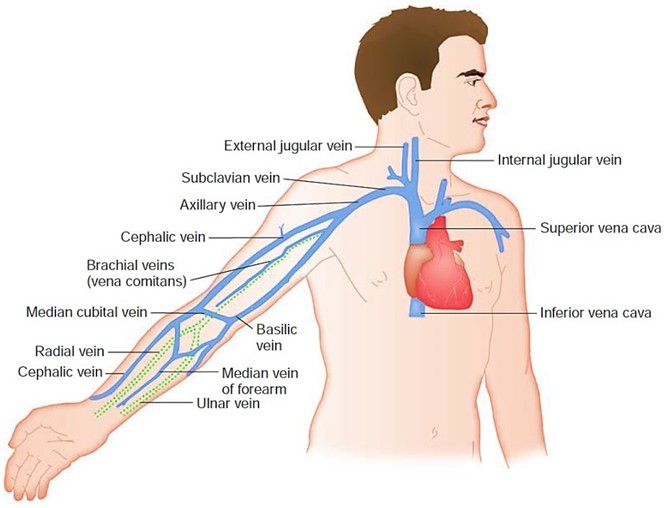
Choice A Reason: This choice is incorrect because administering a vasodilator medication may lower the blood pressure and worsen the cerebral perfusion. A vasodilator medication is a drug that relaxes the blood vessels and reduces the resistance to blood flow. It may be used for clients who have hypertension, angina, or heart failure, but it does not help to reduce the intracranial pressure (ICP).
Choice B Reason: This choice is correct because elevating the head of the bed to 30° may help to improve the venous drainage and decrease the ICP. ICP is the pressure exerted by the brain tissue, cerebrospinal fluid (CSF), and blood within the cranial cavity. A normal ICP range is 5 to 15 mm Hg, and an elevated ICP (>20 mm Hg) can cause cerebral ischemia, herniation, or death. Therefore, positioning the client in a semi-Fowler's position (30° angle) or high- Fowler's position (60° to 90° angle) can facilitate breathing and prevent further complications.
Choice C Reason: This choice is incorrect because applying a cold compress to the forehead may cause vasoconstriction and increase the ICP. A cold compress is a device that applies cold temperature to a body part to reduce inflammation, pain, or swelling. It may be used for clients who have headaches, sprains, or bruises, but it does not help to reduce the ICP.
Choice D Reason: This choice is incorrect because decreasing the oxygen flow rate may cause hypoxia and worsen the cerebral ischemia. Hypoxia is a condition in which the body or a part of it does not receive enough oxygen. It may cause symptoms such as confusion, agitation, or cyanosis. Therefore, providing adequate oxygenation and ventilation is essential to maintain the brain function and prevent further damage.
Correct Answer is D
Explanation
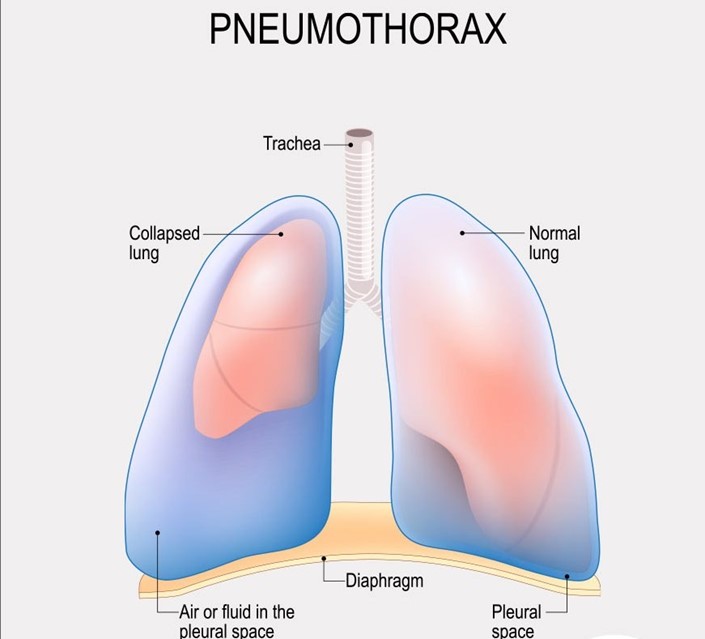
Choice A Reason: This is incorrect because crepitus in the area above and surrounding the insertion site is not a serious finding that requires notification of the provider. Crepitus is a crackling sensation that occurs when air leaks into the subcutaneous tissue. It is usually harmless and resolves on its own.
Choice B reason: This is incorrect because bubbling of the water in the water seal chamber with exhalation is a normal finding that indicates that air is being removed from the pleural space. Bubbling should stop when the pneumothorax is resolved.
Choice C Reason: This is incorrect because eyelets are not visible is not a serious finding that requires notification of the provider. Eyelets are small holes at the end of the chest tube that allow air and fluid to drain from the pleural space. They are usually covered by a dressing and may not be visible.
Choice D Reason: This is correct because movement of the trachea toward the unaffected side is a serious finding that indicates a tension pneumothorax, which is a life-threatening condition that occurs when air accumulates in the pleural space and causes pressure on the mediastinum. The nurse should notify the provider immediately and prepare for needle decompression or chest tube insertion.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
