A nurse is interpreting a client's ECG strip. Which of the following components of the ECG should the nurse examine to determine the time it takes for ventricular depolarization and repolarization?
QRS complex
QT interval
ST segment
PR interval
The Correct Answer is B
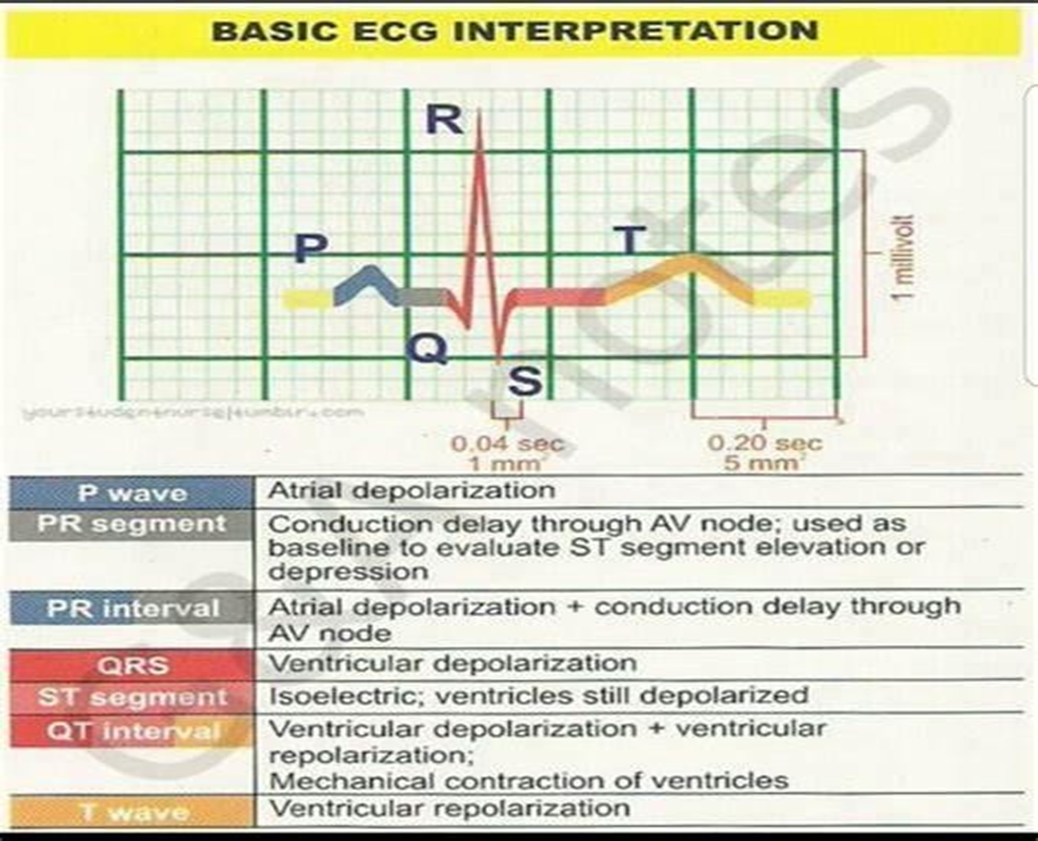
B. The QT interval represents ventricular depolarization and repolarization. It starts at the beginning of the QRS complex and ends at the end of the T wave. The QT interval reflects the total time it takes for both ventricular depolarization and repolarization to occur. Prolongation of the QT interval can be associated with an increased risk of arrhythmias, including torsades de pointes.
A. The QRS complex represents ventricular depolarization, which is the electrical activation of the ventricles. The duration of the QRS complex provides information about the time it takes for ventricular depolarization to occur. A prolonged QRS complex can indicate abnormalities in ventricular conduction, such as bundle branch blocks or ventricular hypertrophy.
C. The ST segment represents the early part of ventricular repolarization. It starts at the end of the QRS complex and ends at the beginning of the T wave. Changes in the ST segment, such as elevation or depression, can indicate myocardial ischemia or injury.
D. The PR interval represents the time it takes for the electrical impulse to travel from the atria to the ventricles. It includes atrial depolarization, atrial contraction, and the delay at the atrioventricular node. The PR interval does not specifically provide information about ventricular depolarization and repolarization.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
A. Dobutamine is a positive inotropic agent that increases myocardial contractility, leading to improved cardiac output. Enhanced cardiac output can result in improved renal perfusion and increased urine output, which is a positive indicator of improved cardiac function in clients with heart failure.
B. Decreased blood glucose level is not typically associated with the effectiveness of dobutamine. Dobutamine primarily affects cardiac contractility and does not directly influence blood glucose levels.
C. Decreased blood pressure would not typically indicate the effectiveness of dobutamine. While dobutamine can increase cardiac output, it does not necessarily lead to a decrease in blood pressure.
D. Increased heart rate may occur as a compensatory mechanism in response to increased cardiac output due to dobutamine administration. However, increased heart rate alone may not reliably indicate the effectiveness of dobutamine.
Correct Answer is C
Explanation
C. The first intervention should be to administer normal saline IV at 500 mL/hr to address the immediate concern of hypotension and inadequate tissue perfusion.
A. While fever control is important, especially in septic shock, administering acetaminophen should not be the first intervention in a patient with severe hypotension and shock. Addressing the low blood pressure and perfusion is a higher priority.
B. Hyperglycemia is common in critically ill patients, including those with septic shock. However, in this scenario, the patient's severely low blood pressure and signs of shock take precedence over managing hyperglycemia. Insulin therapy can be initiated later once the patient's hemodynamic status is stabilized.
D. Norepinephrine is a vasopressor medication commonly used in septic shock to increase blood pressure and improve perfusion to vital organs. It helps counteract the vasodilation and hypotension characteristic of septic shock.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
