A nurse is planning care for a child who has epiglottitis. Which of the following actions should the nurse plan to take?
Obtain a throat culture.
Visualize the epiglottis using a tongue depressor.
Provide moist air to reduce the inflammation of the epiglottis
Initiate airborne precautions.
The Correct Answer is C
A. Obtain a throat culture.
This option is not appropriate as a primary nursing action in the acute management of epiglottitis. While obtaining a throat culture may be necessary for diagnostic purposes, it is not a priority in the immediate care of a child with suspected epiglottitis. The focus should be on ensuring airway patency and providing emergency treatment.
B. Visualize the epiglottis using a tongue depressor.
This option is contraindicated in the acute management of epiglottitis. Direct visualization of the epiglottis using a tongue depressor or other instruments can provoke spasm of the epiglottis and worsen airway obstruction. Attempting to visualize the epiglottis should be avoided until the child's airway has been secured in a controlled environment, such as in the operating room under anesthesia.
C. Provide moist air to reduce the inflammation of the epiglottis.
This option is appropriate. Providing moist air, such as humidified oxygen or a cool mist, can help soothe the inflamed tissues of the epiglottis and upper airway. Moist air may help alleviate discomfort and reduce inflammation, although it will not directly address the risk of airway obstruction. It is often used as supportive therapy in conjunction with other interventions.
D. Initiate airborne precautions.
This option is not necessary for the care of a child with epiglottitis. Epiglottitis is not typically transmitted through airborne droplets. The priority in the management of epiglottitis is ensuring a patent airway and providing appropriate treatment to reduce inflammation and prevent complications.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
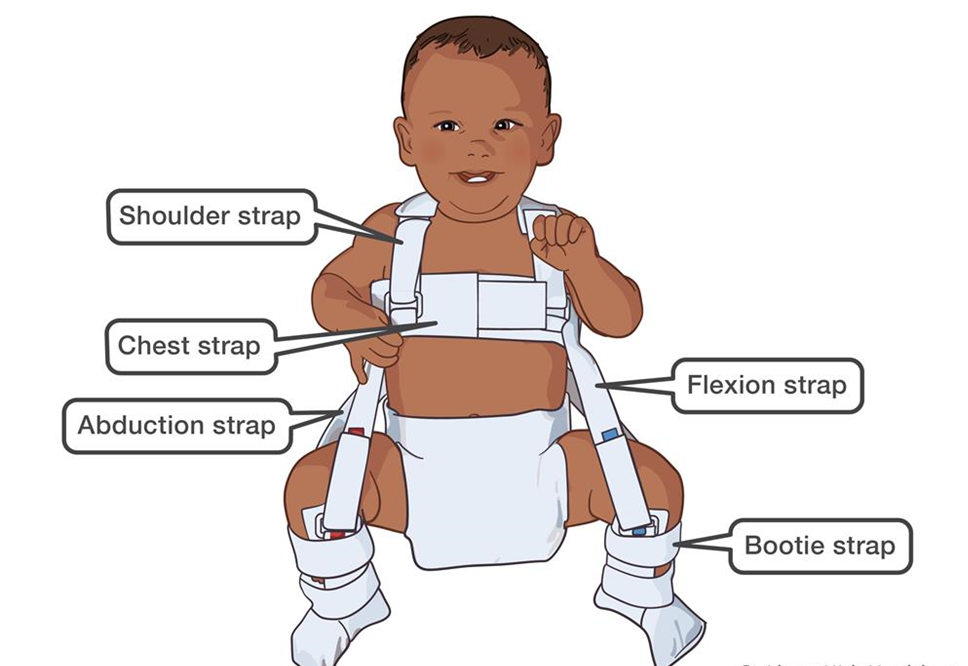
A. "I will use powders & lotion on his skin around the harness clasps."
This statement indicates a misunderstanding. Powders and lotions should generally be avoided around the harness clasps because they can interfere with the proper fit of the harness and cause irritation or discomfort to the baby's skin.
B. “I will remove the harness daily, prior to giving the bath.”
This statement is incorrect. The Pavlik harness is typically not removed for bathing, as it needs to be worn continuously to maintain proper positioning of the hips and promote optimal healing. Removing the harness daily for bathing can disrupt the treatment process and delay progress.
C. "I will adjust the harness straps every day."
This statement indicates a misunderstanding. The harness should not be adjusted daily without guidance from the healthcare provider. The straps of the Pavlik harness are initially adjusted by the healthcare provider to ensure proper fit, and they should remain in place without frequent adjustments to maintain stability and effectiveness.
D. "I will check my baby's skin under the straps frequently."
This statement indicates an understanding of the teaching. It is essential for the mother to regularly check her baby's skin under the harness straps for any signs of irritation, redness, or pressure sores. Monitoring the skin closely allows for early detection of any issues that may arise from wearing the harness.
Correct Answer is D
Explanation
A. Instruct the client to cough. Coughing is generally encouraged after chest physiotherapy to help expel loosened secretions, but it is not the first action. The bronchodilator should be administered first to maximize the effectiveness of the chest physiotherapy.
B. Perform vibration while the client exhales slowly through the nose. Vibration is a component of chest physiotherapy used to help loosen secretions during exhalation, but it is performed after the bronchodilator is administered and once the client is positioned properly.
C. Percuss the upper posterior chest.Percussion helps to mobilize secretions but is typically done after the bronchodilator has been administered to allow for more effective airway clearance.
D. Administer albuterol by nebulizer.Administering albuterol first dilates the airways, making it easier to mobilize and clear secretions during percussion, vibration, and postural drainage.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
