A nurse is planning care for a client who has undergone cardiac catheterization through the femoral artery. Which of the following actions should the nurse plan to take?
Instruct the client to perform range-of-motion exercises to his lower extremities.
Ambulate the client 1 hour following the procedure.
Restrict the client's fluid intake.
Assess the color, temperature, and pulse in the affected extremity.
The Correct Answer is D
Choice A reason: Instructing the client to perform range-of-motion exercises to his lower extremities immediately after cardiac catheterization is not recommended. The client should maintain bed rest with the affected leg straight to prevent bleeding from the catheter insertion site.
Choice B reason: Ambulating the client 1 hour following the procedure is not advised. After femoral artery access, the client is typically required to remain on bed rest with the affected leg straight for several hours to ensure hemostasis and prevent bleeding².
Choice C reason: Restricting the client's fluid intake is not a standard post-procedure action. Adequate hydration is important after cardiac catheterization to help flush the contrast dye used during the procedure from the body, unless contraindicated.
Choice D reason: Assessing the color, temperature, and pulse in the affected extremity is crucial for detecting signs of bleeding, hematoma formation, or arterial occlusion. These assessments should be performed regularly as part of post-cardiac catheterization care².
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
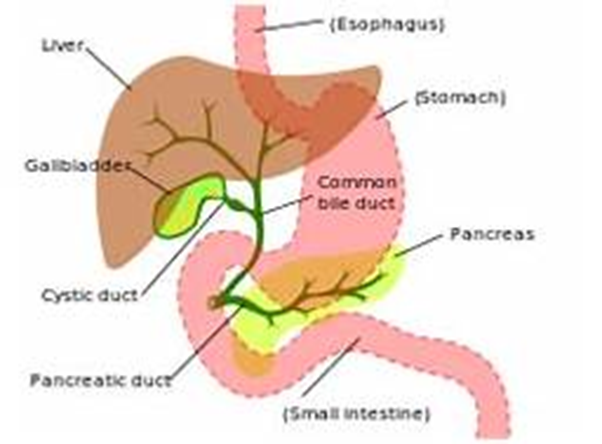
Choice A reason: Tenderness in the left upper abdomen is not typically associated with an obstruction of the common bile duct. This symptom is more commonly related to conditions affecting the stomach, pancreas, or spleen. The common bile duct is in the right upper quadrant of the abdomen, and tenderness in this area might be expected with its obstruction.
Choice B reason: Ecchymosis of the extremities is not a common finding in common bile duct obstruction. Ecchymosis, or bruising, is usually due to trauma, blood disorders, or other causes of fragile blood vessels and is not related to bile duct issues.
Choice C reason: Pale-colored urine is the opposite of what might be expected with common bile duct obstruction. Typically, the urine may become dark due to increased bilirubin levels that are excreted by the kidneys when the bile duct is obstructed.
Choice D reason: Fatty stools, or steatorrhea, are a classic finding in common bile duct obstruction. When bile flow is blocked, fats are not properly digested and absorbed, leading to stools that are bulky, greasy, and often have a foul odor. This occurs because bile is necessary for the emulsification and absorption of dietary fats in the intestine.
Correct Answer is D
Explanation
Choice A reason: Hypermagnesemia, or high levels of magnesium in the blood, is not typically associated with refeeding syndrome. Instead, refeeding syndrome can lead to hypomagnesemia, which is a low level of magnesium in the blood, due to shifts of magnesium into the cells during insulin secretion in the refeeding process.
Choice B reason: Hyponatremia, or low levels of sodium in the blood, is not a hallmark of refeeding syndrome. While fluid shifts can affect sodium levels, the key electrolyte disturbances in refeeding syndrome involve phosphorus, potassium, and magnesium.
Choice C reason: Hyperkalemia, or high levels of potassium in the blood, is not a common finding in refeeding syndrome. Similar to magnesium, potassium can shift into cells during refeeding, which can actually lead to hypokalemia, or low levels of potassium in the blood.
Choice D reason: Hypophosphatemia, or low levels of phosphorus in the blood, is the hallmark of refeeding syndrome. When a malnourished individual is refed, insulin secretion is stimulated by the increased carbohydrate intake. Insulin promotes cellular uptake of glucose, which is accompanied by phosphate, potassium, and magnesium, leading to a decrease in the serum levels of these electrolytes. Phosphorus is critical for cellular processes, and its deficiency can lead to muscle weakness, respiratory failure, hemolysis, and impaired cardiac function. During refeeding, careful monitoring of electrolytes is essential to prevent and manage refeeding syndrome. Hypophosphatemia is the most significant laboratory finding to anticipate in a patient with refeeding syndrome, and it requires prompt recognition and treatment to prevent serious complications.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
