A nurse is teaching a client who is newly diagnosed with type 1 diabetes mellitus about insulin safety. Which of the following statements by the nurse is appropriate?
Insulin is stable at room temperature for one month.
Insulins can be mixed in the same syringe.
Storing insulin in the freezer will prolong its stability.
Clients with type 1 diabetes mellitus should keep backup medication and supplies in their car.
The Correct Answer is A
The correct answer is a. Insulin is stable at room temperature for one month.
Choice A Reason:
Insulin is stable at room temperature (between 59°F and 86°F) for up to one month. This is important for patients to know, especially if they do not have immediate access to refrigeration. However, it is crucial to avoid exposing insulin to extreme temperatures, such as direct sunlight or freezing conditions, as these can degrade the medication’s effectiveness.
Choice B Reason:
While some types of insulin can be mixed in the same syringe, this practice is not universally applicable to all insulin types. For example, rapid-acting and intermediate-acting insulins can sometimes be mixed, but long-acting insulins should not be mixed with other insulins. Therefore, this statement is not entirely accurate and should be clarified based on the specific types of insulin being used.
Choice C Reason:
Storing insulin in the freezer is not recommended as freezing can damage the insulin, rendering it ineffective. Insulin should be stored in a refrigerator at temperatures between 36°F and 46°F. If insulin is accidentally frozen, it should not be used.
Choice D Reason:
While it is advisable for clients with type 1 diabetes to have backup medication and supplies, storing them in a car is not recommended due to the potential for extreme temperature fluctuations. Insulin and other diabetes supplies should be kept in a stable, controlled environment to ensure their efficacy.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Choice A reason:
“I need to walk slowly as I lose my balance often” is a significant safety concern for a client with peripheral artery disease (PAD). Balance issues can increase the risk of falls, which can lead to serious injuries, especially in clients with compromised circulation. PAD can cause muscle weakness and pain, which may contribute to balance problems. Reporting this symptom to the provider is crucial for further evaluation and intervention to prevent falls and improve the client’s mobility and safety.
Choice B reason:
“I have a small-healed area on my spine that is painful” is not directly related to peripheral artery disease. While pain in different parts of the body can be concerning, this statement does not indicate an immediate safety risk associated with PAD. However, it is still important for the nurse to document and monitor this symptom, as it could be related to other underlying conditions.
Choice C reason:
“I don’t go out much because of the pain in my legs” is a common symptom of PAD known as claudication, which is pain caused by too little blood flow during exercise. While this statement indicates a significant impact on the client’s quality of life, it does not pose an immediate safety risk that requires urgent reporting. The nurse should provide education on managing claudication and encourage the client to engage in supervised exercise programs to improve circulation.
Choice D reason:
“It makes me sad that I can’t keep up with my grandchildren” reflects the emotional and psychological impact of PAD on the client’s life. While this is an important aspect of the client’s overall well-being, it does not represent an immediate safety concern. The nurse should address the client’s emotional health and consider referring them to a mental health professional for support.
Correct Answer is ["C","D"]
Explanation
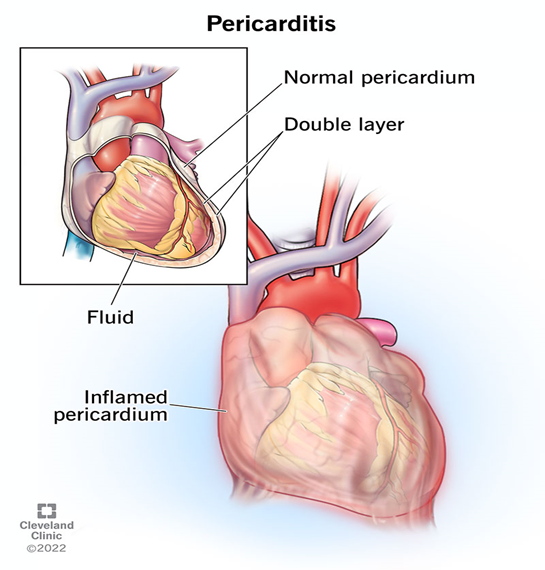
Choice A Reason
Acetaminophen is often used to manage pain and fever, but it is not the primary treatment for pericarditis. While it can help alleviate discomfort, it does not address the inflammation associated with pericarditis12.
Choice B Reason:
Amiodarone is an antiarrhythmic medication used to treat and prevent various types of serious irregular heartbeats, such as ventricular tachycardia or ventricular fibrillation. It is not typically used for treating pericarditis, as it does not address the inflammation or pain associated with the condition.
Choice C Reason:
Colchicine is recommended as part of the first-line treatment for pericarditis. It helps reduce inflammation and the risk of recurrent pericarditis when used in conjunction with NSAIDs5. Colchicine is effective in managing symptoms and preventing recurrences.
Choice D Reason:
Indomethacin is a nonsteroidal anti-inflammatory drug (NSAID) that is effective in reducing inflammation and pain associated with pericarditis. NSAIDs are commonly prescribed for pericarditis to help manage symptoms and reduce inflammation. Indomethacin, along with other NSAIDs like ibuprofen, is often part of the first-line treatment for this condition.
Choice E Reason:
Nitroglycerine is primarily used to treat angina (chest pain) and heart failure by dilating blood vessels and reducing the heart’s workload. It is not typically used for treating pericarditis, as it does not address the inflammation or pain associated with the condition.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
