A nurse is teaching a guardian of a school-age child who has a new prescription for a fluticasone metered-dose inhaler. Which of the following information should the nurse include in the teaching? (Select all that apply.)
"Rinse your child's mouth following administration."
"Have your child take one inhalation as needed for shortness of breath."
"Shake the device prior to administration."
"A spacer will make it easier to use the device."
"Soak the inhaler in water after use
Correct Answer : A,C,D
A. "Rinse your child's mouth following administration." - This is important advice to prevent the development of oral thrush (a fungal infection) and to reduce the risk of irritation in the mouth and throat caused by the medication. After using a fluticasone inhaler, rinsing the mouth with water can help prevent these side effects.
C. "Shake the device prior to administration." - Shaking the inhaler before use ensures proper mixing of the medication and enhances its effectiveness.
D. "A spacer will make it easier to use the device." - A spacer is a device that attaches to the inhaler and helps the medication get into the lungs more effectively, especially for children who might have difficulty coordinating the timing of inhalation with activating the inhaler.
The other options:
B. "Have your child take one inhalation as needed for shortness of breath." - This instruction might not be accurate, as fluticasone is usually used as a maintenance medication to control chronic conditions like asthma. It's not typically used as a rescue inhaler for immediate shortness of breath.
E. "Soak the inhaler in water after use." - Soaking the inhaler in water after use is not a standard practice and is not necessary for proper administration or maintenance.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
A. The nurse who identifies the error:
This choice is correct. When a medication error is identified, the nurse who discovers the error is responsible for completing an incident report. Incident reports are a formal way to document any unexpected or adverse events that occur in a healthcare setting, including medication errors. The report helps track incidents, analyze their causes, and implement preventive measures. It's important for the reporting nurse to provide accurate and detailed information about the error.
B. The Quality Improvement Committee:
This choice is incorrect. While the Quality Improvement (QI) Committee plays a role in analyzing trends, identifying areas for improvement, and developing strategies to enhance patient care quality, they are not typically responsible for completing individual incident reports. The responsibility for reporting and documenting a specific incident, such as a medication error, lies with the staff members directly involved.
C. The charge nurse:
This choice is incorrect. The charge nurse is responsible for overseeing the nursing unit's operations, including staffing and patient care coordination. While the charge nurse may be involved in addressing the situation and ensuring appropriate actions are taken following a medication error, they are not necessarily responsible for completing the incident report. The reporting responsibility usually falls on the nurse who identifies the error.
D. The nurse who caused the error:
This choice is incorrect. While it's important for the nurse who caused the error to communicate the error to appropriate parties and participate in any necessary corrective actions, the primary responsibility for completing the incident report usually lies with the nurse who identifies the error. The reporting nurse's perspective is crucial for understanding the context and details of the error.
Correct Answer is C
Explanation
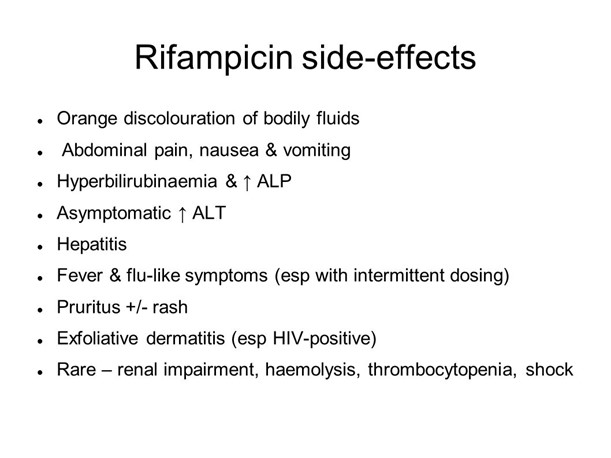
A. Instruct the client to increase his fluid intake: While adequate fluid intake is generally important for various reasons, increasing fluid intake would not alter the orange-red discoloration caused by rifampin. This side effect is due to the drug's action on body fluids, not dehydration.
B. Prepare the client for dialysis: Dialysis is not indicated for the harmless orange-red discoloration caused by rifampin. Dialysis is typically used for clients with kidney failure or significant electrolyte imbalances, and it would not address this specific side effect.
C. Document this as an expected finding.
Explanation:
Rifampin, an antibiotic commonly used in the treatment of tuberculosis (TB), can cause a harmless side effect known as "orange-red discoloration." This can affect bodily fluids such as urine, sweat, and tears. This is not a harmful effect and does not indicate a need for any specific intervention. Therefore, the nurse should document this as an expected finding due to the client's use of rifampin.
D. Check the client's liver function test results: The orange-red discoloration is not related to liver function, so checking liver function test results would not provide relevant information about this particular side effect.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
