A nurse on the labor and delivery unit is planning care for a client who has human immunodeficiency virus (HIV). Which of the following is an appropriate action for the nurse to take following the birth of the newborn?
Cleanse the newborn immediately after delivery.
Initiate contact precautions for the newborn.
Administer intravenous antibiotics to the newborn.
Encourage the mother to breastfeed her newborn.
The Correct Answer is A
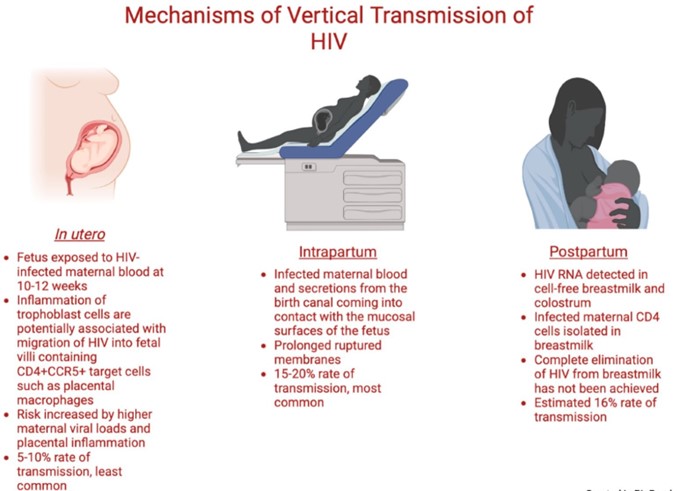
A newborn who is exposed to HIV perinatally should be bathed and cleansed of maternal secretions as soon as possible after birth to reduce the risk of HIV transmission through the skin or mucous membranes¹². The newborn should also receive antiretroviral prophylaxis within six hours of delivery, preferably within two hours¹². The type and duration of prophylaxis depend on the maternal and infant factors that influence the risk of HIV transmission, such as maternal viral load, antiretroviral therapy, mode of delivery, and infant gestational age¹²³. The newborn should also undergo HIV testing at birth, at 14 to 21 days of age, at one to two months of age, and at four to six months of age¹².
The other options are incorrect because:
b) Initiating contact precautions for the newborn is not necessary or recommended. Contact precautions are used to prevent the spread of infections that are transmited by direct or indirect contact with the patient or the patient's environment. HIV is not transmited by casual contact, and standard precautions are sufficient to prevent exposure to blood or body fluids that may contain HIV¹².
c) Administering intravenous antibiotics to the newborn is not indicated for HIV prevention. Antibiotics are used to treat bacterial infections, not viral infections like HIV. Antibiotics may be given to the newborn for other reasons, such as suspected sepsis or chorioamnionitis, but they do not affect the risk of HIV transmission¹².
d) Encouraging the mother to breastfeed her newborn is contraindicated for HIV prevention. Breastfeeding can transmit HIV from the mother to the infant through breast milk, especially if the mother has a high viral load, mastitis, cracked nipples, or oral lesions in the infant. In resource-limited settings where formula feeding may not be feasible or safe, breastfeeding with maternal or infant antiretroviral therapy may be considered, but in developed countries where safe alternatives are available, breastfeeding is not recommended for mothers with HIV infection¹².
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["A","D","E"]
Explanation
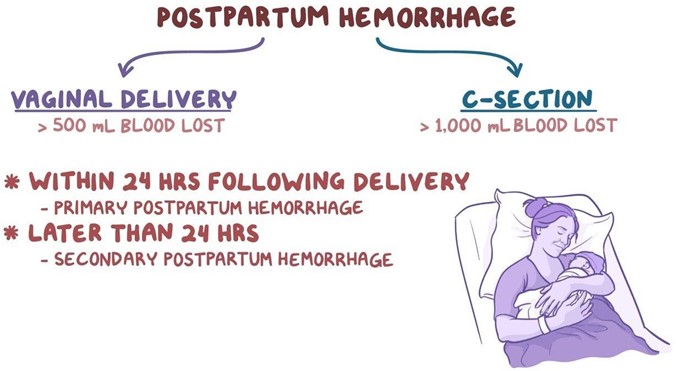
These are the findings that place the client at risk for postpartum hemorrhage. Postpartum hemorrhage (PPH) is severe vaginal bleeding after childbirth. It can be a life-threatening condition that requires prompt treatment. The most common cause of PPH is uterine atony, which is when the uterus does not contract enough to stop the bleeding from the placental site¹. Factors that can increase the risk of uterine atony include:
- History of uterine atony: Having a previous episode of PPH due to uterine atony makes it more likely to
happen again in subsequent deliveries.
- Labor induction with oxytocin: Oxytocin is a hormone that stimulates uterine contractions. However, prolonged or excessive use of oxytocin during labor can cause uterine fatigue and reduce its ability to contract after delivery.
- Vacuum-assisted delivery: A vacuum extractor is a device that helps deliver the baby by applying suction to the baby's head. This can cause trauma to the uterus and increase the risk of bleeding.
The other options are not correct because they are not risk factors for postpartum hemorrhage. Let me
explain why:
b) History of human papillomavirus
Human papillomavirus (HPV) is a common sexually transmited infection that can cause genital warts and cervical cancer. However, it does not increase the risk of postpartum hemorrhage. HPV may affect the cervix, but not the uterus or the placenta, which are the main sources of bleeding after delivery³.
c) Newborn weight 2.948 kg (6 Ib 8 oz)
This is a normal newborn weight and does not increase the risk of postpartum hemorrhage. A large baby (more than 4 kg or 8.8 Ib) may increase the risk of uterine atony by overdistending the uterus, but this is not the case for this newborn².
Correct Answer is A
Explanation
Maternal hypotension is a common complication of spinal anesthesia for cesarean section, and it can cause adverse effects on the mother and the fetus, such as nausea, vomiting, dizziness, decreased placental perfusion, fetal acidosis, and fetal distress¹². To prevent or treat maternal hypotension, various techniques have been used, such as fluid preloading or co-loading, vasopressors, lower limb compression devices, and left lateral tilt position¹². Among these, fluid administration is the most widely used and recommended
intervention¹²³. A bolus infusion of lactated Ringer's or other crystalloid solution can increase the intravascular volume and cardiac output, and counteract the decrease in blood pressure caused by spinal anaesthesia¹²³. The optimal timing and amount of fluid administration may vary depending on the individual patient's condition and response, but generally a bolus of 10 to 20 mL/kg is suggested before or during spinal anaesthesia¹²³.
The other options are incorrect because:
b) Applying oxygen via nonrebreather face mask at 2 L/min is not an effective intervention for maternal hypotension. Oxygen supplementation may be beneficial for improving fetal oxygenation in case of fetal distress, but it does not directly increase maternal blood pressure or cardiac output¹². Moreover, 2 L/min is a low flow rate for a nonrebreather face mask, which requires at least 10 L/min to deliver high concentrations of oxygen⁴.
c) Positioning the client in a knee-chest position is not a recommended intervention for maternal hypotension. This position may increase venous return and cardiac output in some cases, but it also increases intra-abdominal pressure and reduces uterine blood flow, which can compromise fetal oxygenation and well-being. A left lateral tilt position of 15 to 30 degrees is preferred to avoid aortocaval compression and improve placental perfusion¹².
d) Giving terbutaline subcutaneously is not an appropriate intervention for maternal hypotension. Terbutaline is a beta-agonist that relaxes the uterine smooth muscle and prevents preterm labor contractions. It has no direct effect on maternal blood pressure or cardiac output, and it may cause maternal tachycardia, palpitations, tremors, and hypokalemia as side effects. Vasopressors such as ephedrine or phenylephrine are more effective and safer drugs for treating maternal hypotension¹².

Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
