A nurse is caring for a client who is 1 day postpartum and breastfeeding her newborn. The client reports sore nipples. Which of the following actions should the nurse take?
Instruct the client to wait 4 hours between daytime feedings.
Offer supplemental formula between the newborn's feedings.
Have the client limit the length of breastfeeding to 5 minutes per breast.
Assess the newborn's latch while breastfeeding.
Assess the newborn's latch while breastfeeding.
The Correct Answer is D
Sore nipples are a common problem for breastfeeding mothers, especially in the first few days or weeks after delivery. They can cause pain, discomfort, and frustration, and may interfere with breastfeeding success and satisfaction. The most common cause of sore nipples is poor latch, which means that the newborn does not attach to the breast correctly and does not suckle effectively. Poor latch can result from various factors, such as improper positioning, tongue-tie, inverted or flat nipples, engorgement, or thrush.
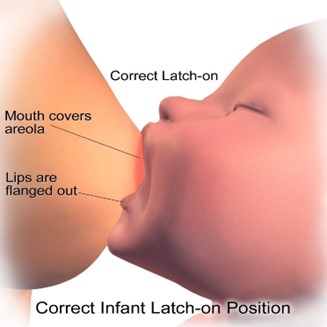
The nurse should assess the newborn's latch while breastfeeding to identify and correct any problems that may cause sore nipples. The nurse should observe the following signs of a good latch:
- The newborn's mouth is wide open and covers most of the areola (the dark area around the nipple).
- The newborn's chin and nose touch the breast, and the cheeks are rounded and not dimpled.
- The newborn's tongue is visible under the lower lip and curls around the breast.
- The newborn's lips are flanged outwards and not tucked inwards.
- The newborn's jaw moves rhythmically and smoothly, and swallowing sounds are audible.
- The mother feels a gentle tugging sensation on the nipple, but no pain or pinching.
The nurse should also teach the mother how to achieve a good latch by using different positions, supporting the breast with her hand, tickling the newborn's lower lip with her nipple, and bringing the newborn to the breast when their mouth is wide open. The nurse should also encourage the mother to seek help from a lactation consultant or a peer support group if she has persistent or severe nipple pain.
a) Instructing the client to wait 4 hours between daytime feedings is not an appropriate action for the nurse to take. This may reduce nipple soreness temporarily, but it can also cause breast engorgement, milk supply reduction, mastitis, or poor weight gain in the newborn. The nurse should advise the client to feed the newborn on demand, usually every 1.5 to 3 hours during the day and every 3 to 4 hours at night.
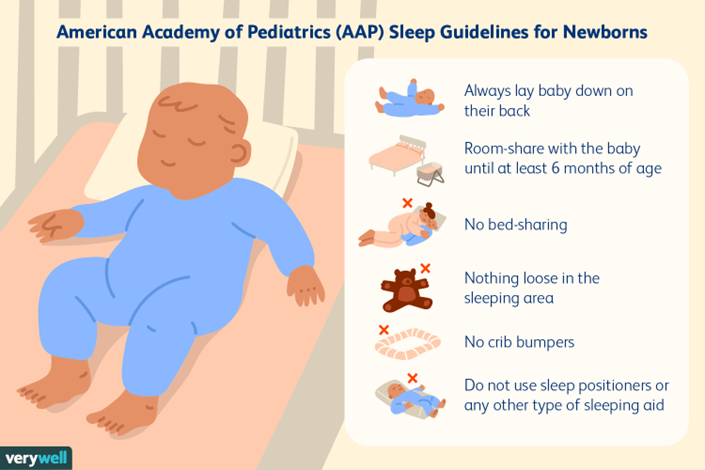
b) Offering supplemental formula between the newborn's feedings is not an appropriate action for the nurse to take. This may interfere with breastfeeding initiation and establishment, as it can reduce the mother's milk supply, confuse the newborn's sucking pattern, increase the risk of nipple preference or rejection, and expose the newborn to potential allergens or infections. The nurse should support exclusive breastfeeding for the first six months of life, unless there is a medical indication for supplementation.
c) Having the client limit the length of breastfeeding to 5 minutes per breast is not an appropriate action for the nurse to take. This may not be enough time for the newborn to get enough milk, especially the hindmilk that is richer in fat and calories. It may also prevent proper drainage of the breast and lead to engorgement or mastitis. The nurse should advise the client to let the newborn feed until they are satisfied and release the breast on their own, which may take 10 to 20 minutes per breast on average.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
When reviewing infection control procedures in a newborn nursery, the nurse manager should instruct the newly hired nurses to place newborn bassinets at least 3 feet apart. This practice helps prevent the spread of infections between infants by minimizing close contact and reducing the risk of droplet transmission.
Option a) Maintaining airborne precautions in the nursery is not necessary unless there is a specific airborne infectious disease outbreak or a newborn with a known airborne infection. Standard precautions, including hand hygiene and proper use of personal protective equipment, are generally sufficient to prevent the spread of infections in a newborn nursery.
Option b) Placing the newborn's foot on a sterile field during a heelstick is not necessary for routine procedures. However, a clean and disinfected surface should be used to perform the heelstick to minimize the risk of introducing pathogens. Sterile fields are typically reserved for sterile procedures in an operating room or other controlled environments.
Option d) Allowing parents to enter the nursery if they are wearing a mask is not a standard infection control practice. In general, only authorized personnel should enter the nursery, and parents or visitors should follow any specific visiting policies in place. If there are concerns about respiratory infections or outbreaks, additional visitor restrictions or requirements may be implemented.
Correct Answer is A
Explanation
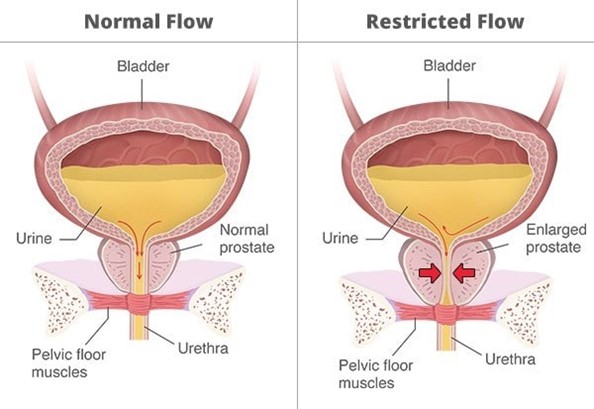
Bladder distention is a common postpartum complication that can occur due to decreased bladder sensation, perineal edema, trauma, or pain after vaginal birth. Bladder distention can interfere with uterine contraction and involution, leading to increased bleeding and risk of infection. Therefore, it is important to assess and manage bladder distention promptly and effectively in postpartum clients.
The first action the nurse should take for a client who has bladder distention is to assist the client to the bathroom and encourage voiding. This is the least invasive and most natural way to empty the bladder and relieve the distention. The nurse should provide privacy, comfort, and support to the client, and help with perineal care after voiding. The nurse should also measure the urine output and monitor for signs of urinary retention or infection, such as dribbling, frequency, urgency, dysuria, hematuria, or foul-smelling urine.
b) Inserting a urinary catheter is not the first action the nurse should take for a client who has bladder distention. A urinary catheter is an invasive procedure that can introduce infection, trauma, or irritation to the urinary tract. It should be used only as a last resort when other methods of bladder emptying have failed or are contraindicated. The nurse should obtain a provider's order before inserting a urinary catheter and follow strict aseptic technique.
c) Offering the client a sitz bath is not the first action the nurse should take for a client who has bladder distention. A sitz bath is a warm water bath that covers only the hips and buttocks. It can provide comfort and promote healing for clients who have perineal lacerations, episiotomies, or hemorrhoids after vaginal birth. However, it does not directly address bladder distention or facilitate voiding. It may also increase the risk of infection or bleeding if done too soon or too frequently after delivery.
d) Pouring warm water over the client's perineum is not the first action the nurse should take for a client who has bladder distention. Pouring warm water over the perineum can help with perineal care and hygiene after vaginal birth. It can also stimulate voiding by creating a relaxing effect on the pelvic floor muscles. However, it does not ensure complete bladder emptying or relieve bladder distention. It may also cause discomfort or irritation if the water temperature or pressure is too high.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
