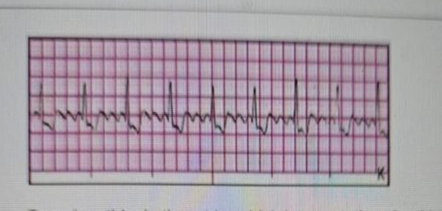
Based on this rhythm strip, which interpretation should the nurse make?
Junctional tachycardia.
Second degree Type II atrioventricular (AV) block (3 to 1).
Ventricular fibrillation.
Atrial flutter.
The Correct Answer is D
A. Junctional tachycardia: Junctional tachycardia originates from the AV node, typically with a narrow QRS, absent or inverted P waves, and a rate of 100–180 bpm. The strip does not show these features.
B. Second-degree Type II AV block (3:1).Type II AV block (Mobitz II) shows dropped QRS complexes with constant PR intervals before conducted beats. This strip does not show missing QRS complexes in a 3:1 pattern.
C. Ventricular fibrillation. VF is characterized by a chaotic, disorganized rhythm with no discernible P waves, QRS complexes, or T waves, completely different from this organized flutter pattern.
D. Atrial flutter is characterized by regular, rapid atrial depolarizations (flutter waves) at a rate of 250–350 bpm. These waves create a "sawtooth" pattern on the ECG.The ventricular response may be regular or irregular, depending on AV conduction. This is different from atrial fibrillation (which has irregularly irregular R-R intervals and no discrete P waves).
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
A. Administer famotidine 20 mg IV. Famotidine is a histamine-2 receptor antagonist used for stress ulcer prophylaxis in critically ill patients. While this medication may be beneficial, it is not the priority intervention based on the insulin protocol and the client's blood glucose level.
B. Titrate insulin infusion by 1 unit/hour. The client’s blood glucose is 160 mg/dL, which falls within the 150–199 mg/dL range according to the insulin protocol. The protocol directs the nurse to increase the insulin drip rate by 1 unit/hour to maintain blood glucose levels below 150 mg/dL. This is the most immediate and appropriate action.
C. Increase dopamine 2 mcg/kg. The client’s MAP is 66 mmHg, which meets the protocol goal of keeping MAP >65 mmHg. There is no indication for increasing dopamine at this time, as the blood pressure is already within the target range.
D. Raise oxygen by 10 percent. The client is on 50% FiO₂ via a face mask with an oxygen saturation of 92%, which is adequate oxygenation for a critically ill patient. Increasing FiO₂ unnecessarily may contribute to oxygen toxicity and is not required based on current oxygenation status.
Correct Answer is D
Explanation
A. Heparin is infused in less than four hours. The heparinized solution used in an intra-arterial (IA) pressure infuser is not intended for systemic anticoagulation but rather to maintain catheter patency. The infusion rate is typically slow and continuous, and completing the infusion in less than four hours is not an indicator of effectiveness.
B. Systolic blood pressure greater than 120 mm Hg. Heparin in an IA pressure infuser does not directly affect blood pressure. Its purpose is to prevent clot formation within the catheter, ensuring uninterrupted arterial pressure monitoring. BP readings are monitored separately and are not an indicator of heparin’s therapeutic effect.
C. No knee pain upon forced dorsiflexion. This assessment is used to evaluate deep vein thrombosis (DVT) (Homan's sign), which is not related to arterial catheter function. The low-dose heparin in the pressure infuser does not provide systemic anticoagulation, making this finding irrelevant.
D. Intra-arterial cannula remains patent. The primary purpose of heparinized flush solutions in IA lines is to prevent clot formation within the catheter and maintain patency for continuous blood pressure monitoring or arterial blood sampling. A patent arterial line confirms that the heparin infusion is achieving its intended effect.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
