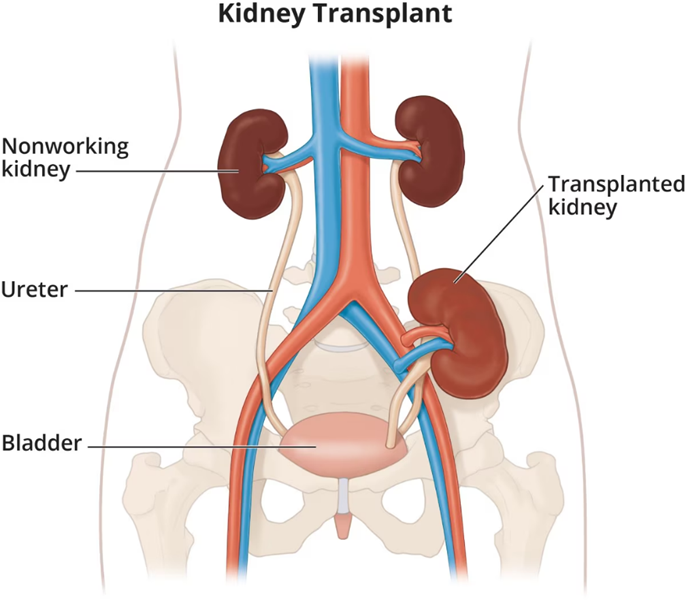
A client who received a renal transplant three months ago is readmitted to the acute care unit with signs of graft rejection. While taking the client’s history, the nurse determines that the client has been self-administering St. John’s Wort, an herbal preparation, on the advice of a friend. Which information is most significant about this finding?
St. John’s Wort can decrease plasma concentrations of cyclosporine.
The client probably used this herb to treat depression.
Ingestion of St. John’s Wort can reduce the client’s intake of sodium.
Adding the herb can decrease the need for corticosteroids.
The Correct Answer is A
Choice A Reason:
St. John’s Wort is known to significantly decrease the blood concentrations of cyclosporine, a critical immunosuppressant used to prevent organ rejection in transplant patients. This herb induces the activity of cytochrome P450 enzymes, particularly CYP3A4, which increases the metabolism of cyclosporine, leading to lower plasma levels and a higher risk of graft rejection. This interaction is highly significant and requires immediate attention to adjust the client’s medication regimen and prevent further complications.
Choice B Reason:
While it is true that St. John’s Wort is commonly used to treat depression, this information is not as significant in the context of graft rejection. The primary concern is the herb’s interaction with cyclosporine, which directly impacts the effectiveness of the immunosuppressive therapy. Understanding the reason for using the herb is important, but it does not address the immediate risk of graft rejection.
Choice C Reason:
There is no substantial evidence to suggest that ingestion of St. John’s Wort reduces sodium intake. This statement does not relate to the herb’s interaction with cyclosporine or its impact on graft rejection. Therefore, it is not a significant concern in this scenario.
Choice D Reason:
Adding St. John’s Wort does not decrease the need for corticosteroids. In fact, the herb’s interaction with cyclosporine can lead to inadequate immunosuppression, potentially increasing the need for additional medications to manage graft rejection. This statement is incorrect and does not address the critical issue of cyclosporine metabolism.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A Reason:
Avoiding taking the medication on an empty stomach is important to reduce gastrointestinal upset. Lithium can cause stomach irritation, and taking it with food can help mitigate this side effect. However, while this is good advice, it is not the most critical instruction to emphasize.
Choice B Reason:
Reporting fluctuations in weight to the healthcare provider is essential because significant weight changes can indicate potential side effects or complications from lithium therapy. Weight gain or loss can be a sign of thyroid dysfunction or other metabolic issues. While important, it is not the primary instruction to emphasize.
Choice C Reason:
Maintaining a fluid intake of 1500 to 2000 mL per day is crucial for clients taking lithium. Lithium levels in the blood can be affected by fluid balance, and dehydration can lead to lithium toxicity. Ensuring adequate hydration helps maintain stable lithium levels and reduces the risk of toxicity. This is the most critical instruction to emphasize to ensure the client’s safety and effective management of their condition.
Choice D Reason:
Keeping medication fliers for frequent review and reference is helpful for understanding the medication and its potential side effects. However, it is not the most critical instruction. The primary focus should be on maintaining proper hydration to prevent lithium toxicity.
Correct Answer is ["200"]
Explanation
Step-by-Step Calculation
Step 1: Determine the total volume to be infused.
- The IV bag contains 200 mL of solution.
Step 2: Determine the infusion time.
- The infusion time is 1 hour.
Step 3: Calculate the infusion rate.
- Infusion rate = Total volume ÷ Infusion time
- Infusion rate = 200 mL ÷ 1 hour
Result: The infusion rate is 200 mL/hr.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
