A nurse is assisting with the care of a client who is in the second stage of labor.
The nurse observes retraction of the fetal head against the maternal perineum as the head is birthed.
Which of the following actions should the nurse take?
Prepare for the delivery of the shoulders.
Encourage the mother to push during the next contraction.
Call for additional medical support.
Administer pain relief medication.
The Correct Answer is A
Choice A rationale:
Normal progression of labor: After the fetal head is delivered, the shoulders typically follow immediately. The nurse should be prepared to assist with the delivery of the shoulders to ensure a safe and smooth birth process.
Significance of retraction: Retraction of the fetal head against the maternal perineum, also known as the "turtle sign," is a classic indicator of shoulder dystocia. While this sign does not guarantee shoulder dystocia, it warrants immediate preparation for potential management.
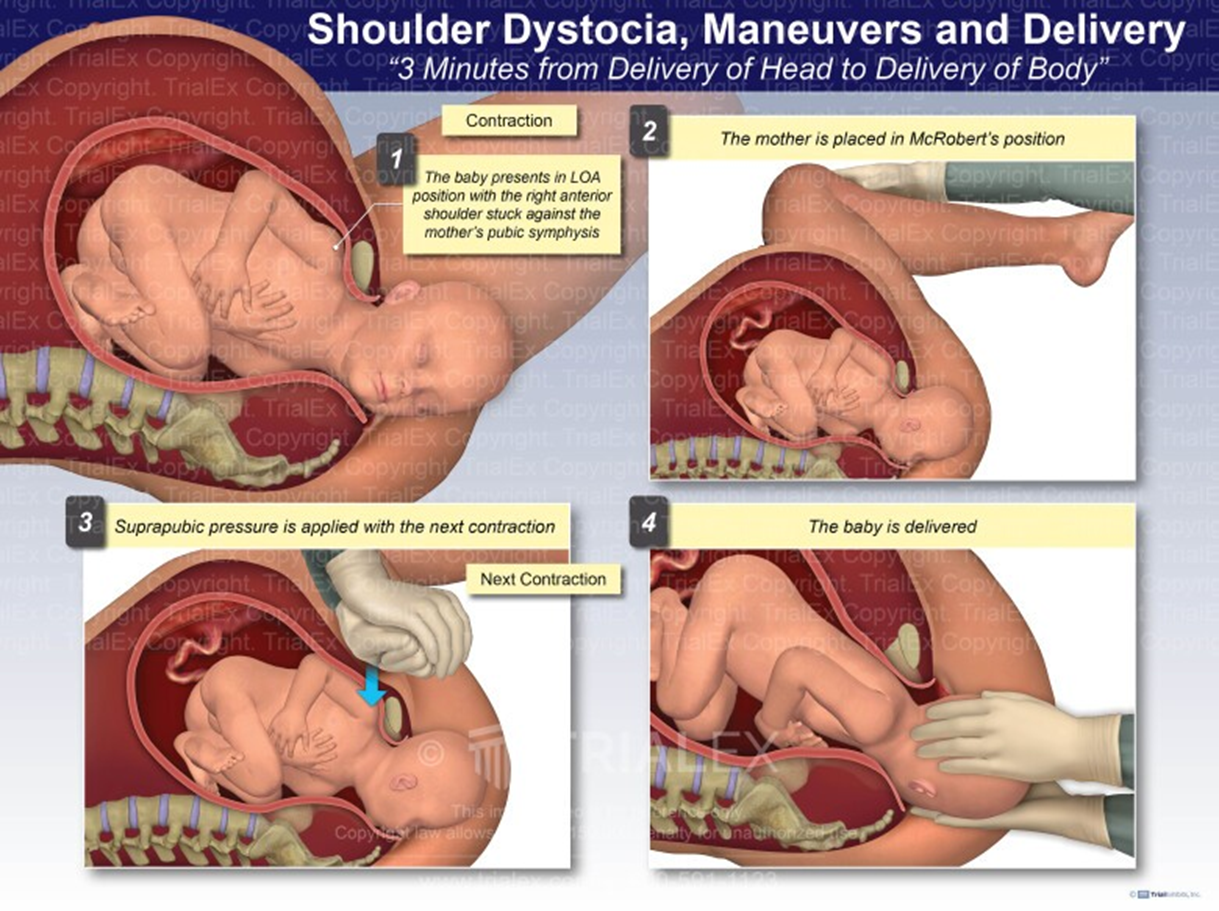
Anticipating shoulder dystocia: By anticipating the possibility of shoulder dystocia, the nurse can take proactive measures to minimize risks and facilitate delivery. These measures may include:
Positioning the mother appropriately (e.g., McRoberts maneuver)
- Applying suprapubic pressure
- Performing internal maneuvers (e.g., Rubin's maneuver)
- Breaking the clavicle (in extreme cases)
Choice B rationale:
Ineffective in shoulder dystocia: Encouraging the mother to push during the next contraction is not an effective intervention
for shoulder dystocia. In fact, excessive pushing can worsen the impaction of the shoulders and potentially lead to
complications such as fetal hypoxia, brachial plexus injury, or maternal perineal trauma.
Choice C rationale:
Necessary in confirmed dystocia: Calling for additional medical support is crucial if shoulder dystocia is confirmed. However,
immediate preparation for shoulder delivery should commence without delay, as prompt action is essential to prevent adverse
outcomes.
Choice D rationale:
Secondary concern: While pain relief medication may be administered for maternal comfort, it is not a priority intervention in
this situation. The primary focus should be on managing the potential shoulder dystocia and ensuring the safe delivery of the
baby.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["A","B","D","E"]
Explanation
Choice A rationale:
Performing hand hygiene before and after voiding is crucial in preventing perineal infection. Hand hygiene is the most
effective way to prevent the spread of infections, including those that can infect the perineum.
Choice B rationale:
Cleaning the perineal area from front to back is a standard recommendation to prevent infection. This method ensures that
bacteria from the anal area are not spread to the vagina and urethra, which can cause urinary tract infections.
Choice C rationale:
Sitting on an inflatable donut is not typically recommended for the prevention of perineal infection. While it can provide
comfort for those with perineal pain, especially after childbirth, it does not directly contribute to the prevention of infection.
Choice D rationale:
Applying ice packs to the perineal area several times daily can help reduce swelling and provide pain relief, especially after a
vaginal birth. While it does not directly prevent infection, it can promote healing and comfort, which can indirectly help
prevent infection.
Choice E rationale:
Blotting the perineal area dry after voiding is another important step in preventing perineal infection. Keeping the area dry
prevents the growth of bacteria and other microbes that thrive in moist environments.
Correct Answer is A
Explanation
Choice A rationale:
Retraction of the fetal head against the maternal perineum is a classic sign that the shoulders are about to be delivered. This is
known as the "turtle sign" because the fetal head appears to retract back into the body like a turtle's head.
It is important for the nurse to be prepared to assist with the delivery of the shoulders to ensure a safe and smooth delivery.
This includes:
Positioning the mother appropriately, such as in the McRoberts maneuver or a hands-and-knees position.
Applying gentle downward traction on the fetal head to help deliver the anterior shoulder.
Rotating the fetal shoulders as needed to facilitate delivery.
Monitoring the fetal heart rate closely for any signs of distress.
Choice B rationale:
While encouraging the mother to rest between contractions is important for conserving energy, it is not the priority action
when the fetal head is retracting. The nurse's focus should be on preparing for the delivery of the shoulders.
Choice C rationale:
Checking the mother's blood pressure is a routine part of labor and delivery care, but it is not specifically indicated when the
fetal head is retracting. There is no evidence to suggest that retraction of the fetal head is associated with changes in maternal
blood pressure.
Choice D rationale:
Administering oxygen to the mother may be helpful in some cases, such as if the fetal heart rate is showing signs of distress.
However, it is not the priority action when the fetal head is retracting. The focus should be on preparing for the delivery of the
shoulders.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
