A nurse is collecting data from a client who is 12 hours postpartum following a spontaneous vaginal delivery.
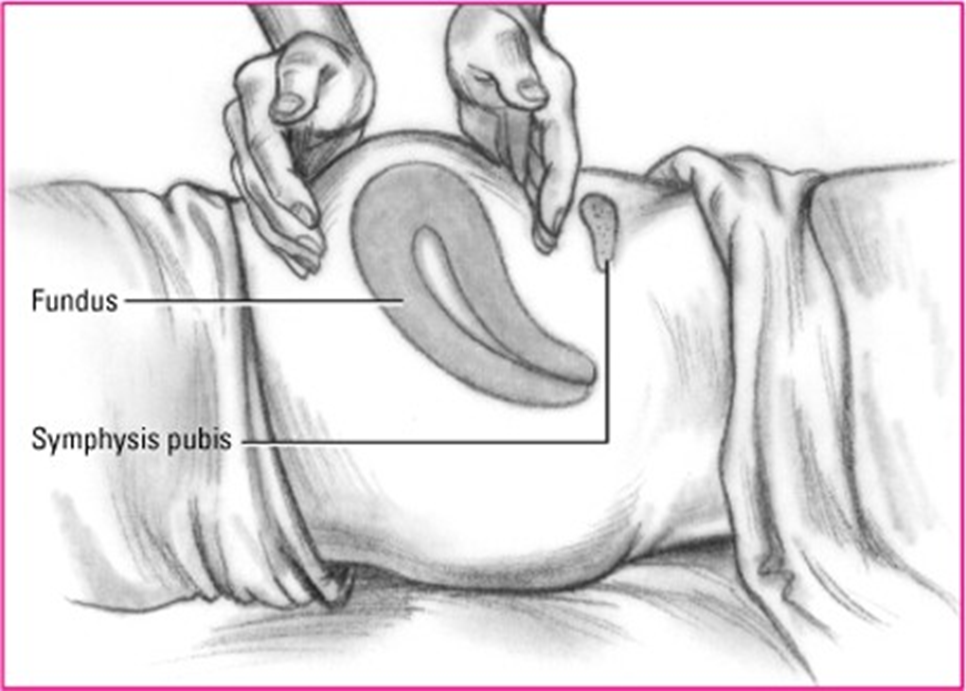
The nurse should expect to find the uterine fundus at which of the following positions on the client’s abdomen?
Three fingerbreadths above the umbilicus
At the level of the umbilicus
One fingerbreadth above the symphysis pubis
One fingerbreadth below the umbilicus
The Correct Answer is B
Choice A rationale:
Three fingerbreadths above the umbilicus is too high for the uterine fundus to be at 12 hours postpartum. Immediately after delivery, the fundus is typically at the level of the umbilicus. It then descends approximately one fingerbreadth per day.
If the fundus is found to be three fingerbreadths above the umbilicus at 12 hours postpartum, it could be a sign of uterine atony, which is a serious condition that can lead to postpartum hemorrhage.
Choice C rationale:
One fingerbreadth above the symphysis pubis is too low for the uterine fundus to be at 12 hours postpartum. This would be more consistent with a woman who is several days postpartum.
Choice D rationale:
One fingerbreadth below the umbilicus is also too low for the uterine fundus to be at 12 hours postpartum. This would be more consistent with a woman who is 1-2 days postpartum.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Choice A rationale:
Normal progression of labor: After the fetal head is delivered, the shoulders typically follow immediately. The nurse should be prepared to assist with the delivery of the shoulders to ensure a safe and smooth birth process.
Significance of retraction: Retraction of the fetal head against the maternal perineum, also known as the "turtle sign," is a classic indicator of shoulder dystocia. While this sign does not guarantee shoulder dystocia, it warrants immediate preparation for potential management.
Anticipating shoulder dystocia: By anticipating the possibility of shoulder dystocia, the nurse can take proactive measures to minimize risks and facilitate delivery. These measures may include:
Positioning the mother appropriately (e.g., McRoberts maneuver)
- Applying suprapubic pressure
- Performing internal maneuvers (e.g., Rubin's maneuver)
- Breaking the clavicle (in extreme cases)
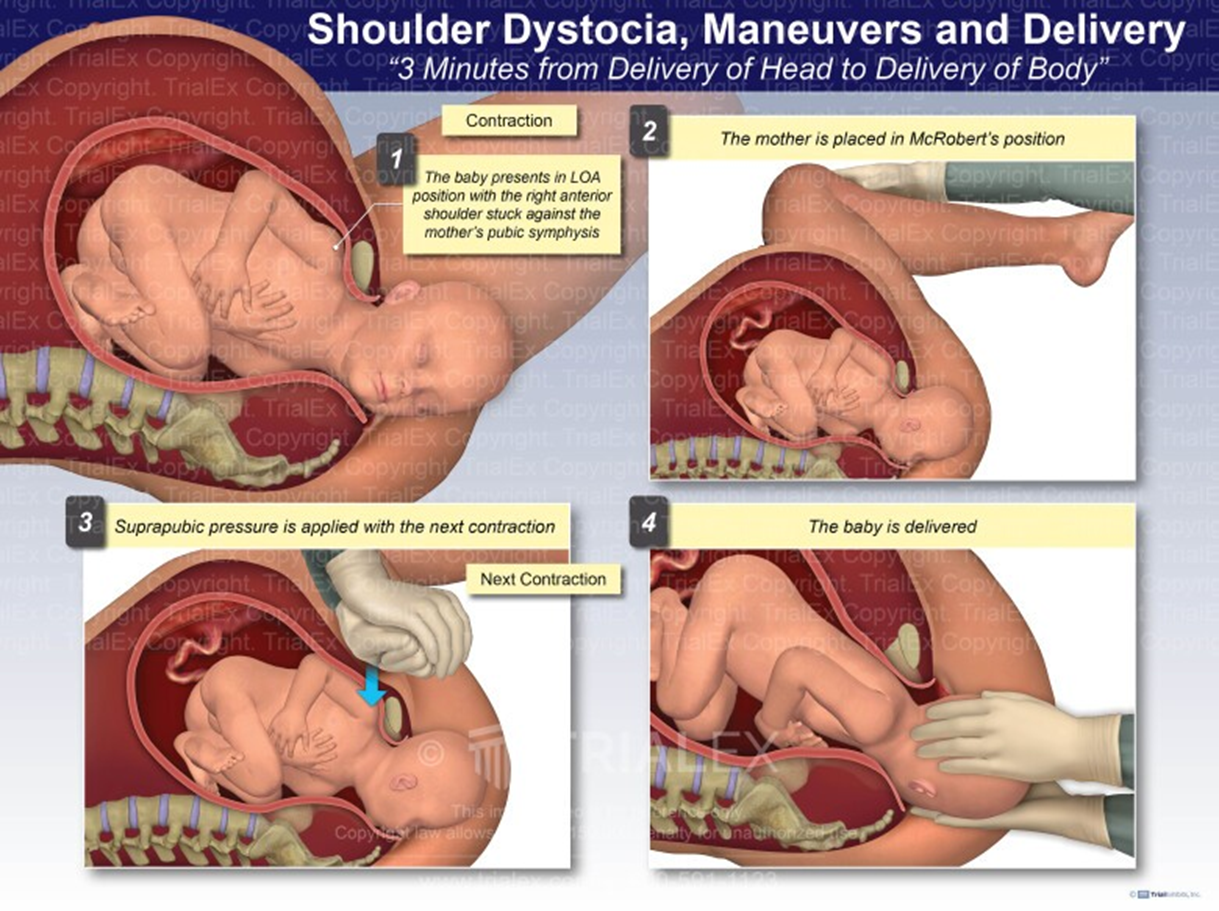
Choice B rationale:
Ineffective in shoulder dystocia: Encouraging the mother to push during the next contraction is not an effective intervention
for shoulder dystocia. In fact, excessive pushing can worsen the impaction of the shoulders and potentially lead to
complications such as fetal hypoxia, brachial plexus injury, or maternal perineal trauma.
Choice C rationale:
Necessary in confirmed dystocia: Calling for additional medical support is crucial if shoulder dystocia is confirmed. However,
immediate preparation for shoulder delivery should commence without delay, as prompt action is essential to prevent adverse
outcomes.
Choice D rationale:
Secondary concern: While pain relief medication may be administered for maternal comfort, it is not a priority intervention in
this situation. The primary focus should be on managing the potential shoulder dystocia and ensuring the safe delivery of the
baby.
Correct Answer is C
Explanation
Choice C rationale:
Monitoring contraction frequency is essential to assess the progression of labor. Contractions are the tightening and relaxing of the uterine muscles that help to dilate the cervix and push the baby down the birth canal. The frequency of contractions is measured in minutes from the beginning of one contraction to the beginning of the next. As labor progresses, contractions become more frequent, regular, and intense. Monitoring contraction frequency helps the nurse to determine the stage of labor, assess the effectiveness of interventions, and identify any potential complications.
Monitoring fetal heart rate is crucial to assess the well-being of the baby during labor. The fetal heart rate is normally between 110 and 160 beats per minute. A normal fetal heart rate indicates that the baby is getting enough oxygen and is not in distress. Variations in the fetal heart rate, such as decelerations or tachycardia, can indicate potential problems and may require intervention.
Choice A rationale:
Preterm labor is defined as labor that begins before 37 weeks of gestation. The client in this scenario is at 38 weeks of gestation, which is considered term. Therefore, preterm labor is not the most likely condition.
Choice B rationale:
The administration of medication and bed rest may be appropriate interventions for preterm labor, but they are not the most appropriate interventions for a client in labor at 38 weeks of gestation. At this stage of pregnancy, labor is considered to be full-term, and interventions are focused on supporting the normal labor process and ensuring the safety of the mother and baby.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
