A nurse is providing discharge teaching to a client who has heart failure. Which of the following lifestyle modifications should the nurse include in the discharge teaching?
Dietary and fluid restrictions
Encouraging increased mobility
Cessation of hormonal supplements
Cessation of intravenous (IV) drug use
None
None
The Correct Answer is A
Choice A: Dietary and Fluid Restrictions
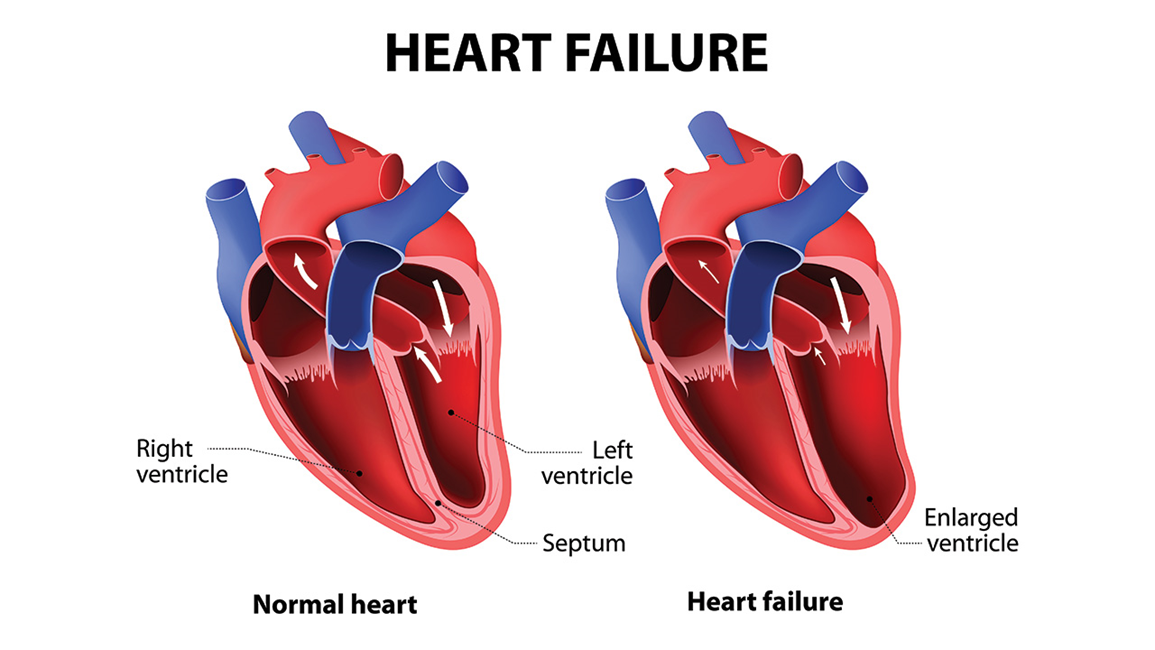
Dietary and fluid restrictions are crucial for patients with heart failure. These restrictions help manage symptoms and prevent complications. Limiting sodium intake can reduce fluid retention, which decreases the workload on the heart. Fluid restrictions help prevent fluid overload, which can lead to worsening heart failure symptoms. Patients are often advised to monitor their weight daily to detect fluid retention early. This choice is essential for managing heart failure effectively.
Choice B: Encouraging Increased Mobility
While physical activity is generally beneficial for overall health, it must be approached cautiously in patients with heart failure. Encouraging increased mobility without proper medical guidance can lead to overexertion and exacerbate heart failure symptoms. Exercise programs for heart failure patients should be tailored and supervised by healthcare professionals to ensure safety and effectiveness. Therefore, this choice is not as immediately critical as dietary and fluid restrictions.
Choice C: Cessation of Hormonal Supplements
Hormonal supplements can have various effects on the cardiovascular system, but their cessation is not a standard recommendation for all heart failure patients. The impact of hormonal supplements depends on the specific type and the patient’s overall health condition. This choice is less relevant compared to dietary and fluid restrictions, which have a direct and significant impact on heart failure management.
Choice D: Cessation of Intravenous (IV) Drug Use
Cessation of intravenous drug use is important for overall health and preventing infections, but it is not specific to heart failure management. While IV drug use can lead to complications that may affect the heart, it is not a primary lifestyle modification recommended for heart failure patients. The focus should be on managing fluid balance and dietary intake
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Choice A: Fasting blood glucose of 140 mg/dL
A fasting blood glucose level of 140 mg/dL is above the normal range (70-99 mg/dL) but may indicate some improvement in beta cell function if it was previously higher. In type 2 diabetes, beta cells in the pancreas are responsible for producing insulin. When beta cells start to restore their function, they can produce more insulin, which helps lower blood glucose levels. However, a fasting blood glucose level of 140 mg/dL still indicates that the client has diabetes and needs to continue managing their condition.
Choice B: Client reports smoking cessation
Smoking cessation is a positive health behavior and can improve overall health, including cardiovascular health, which is often compromised in individuals with diabetes. However, it does not directly indicate the restoration of beta cell function. Beta cell function is specifically related to the pancreas’s ability to produce insulin, and smoking cessation, while beneficial, does not directly impact this.
Choice C: Weight gain of 5 lb
Weight gain can have various implications for a person with type 2 diabetes. While modest weight gain might indicate improved nutritional status or muscle mass, it does not directly indicate the restoration of beta cell function. In fact, weight gain can sometimes worsen insulin resistance, making it harder for beta cells to function effectively.
Correct Answer is D
Explanation
Choice A Reason:
Decreasing activity is not recommended for managing peripheral venous disease. Regular physical activity, such as walking, helps improve blood circulation and can reduce symptoms. Inactivity can lead to worsening of the condition and increase the risk of complications.
Choice B Reason:
Massaging the legs frequently is not typically recommended for preventing fluid buildup in peripheral venous disease. Instead, compression therapy, such as wearing compression stockings, is more effective in managing symptoms and preventing fluid accumulation.
Choice C Reason:
Keeping the legs in a dependent position (hanging down) can worsen symptoms of peripheral venous disease. Elevating the legs above heart level helps reduce swelling and improve blood flow, which is beneficial for managing the condition.
Choice D Reason:
Inspecting the legs daily for changes in color, size, and temperature is crucial for managing peripheral venous disease. This practice helps in early detection of complications such as infections, ulcers, or worsening of the condition, allowing for timely medical intervention.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
