During a skin inspection at the outpatient clinic, the nurse notices patches of thick, red skin with silvery scales on the client's elbows and knees. What skin abnormality does the nurse suspect?
Psoriasis
Rosacea
Scabies
Stasis dermatitis
The Correct Answer is A
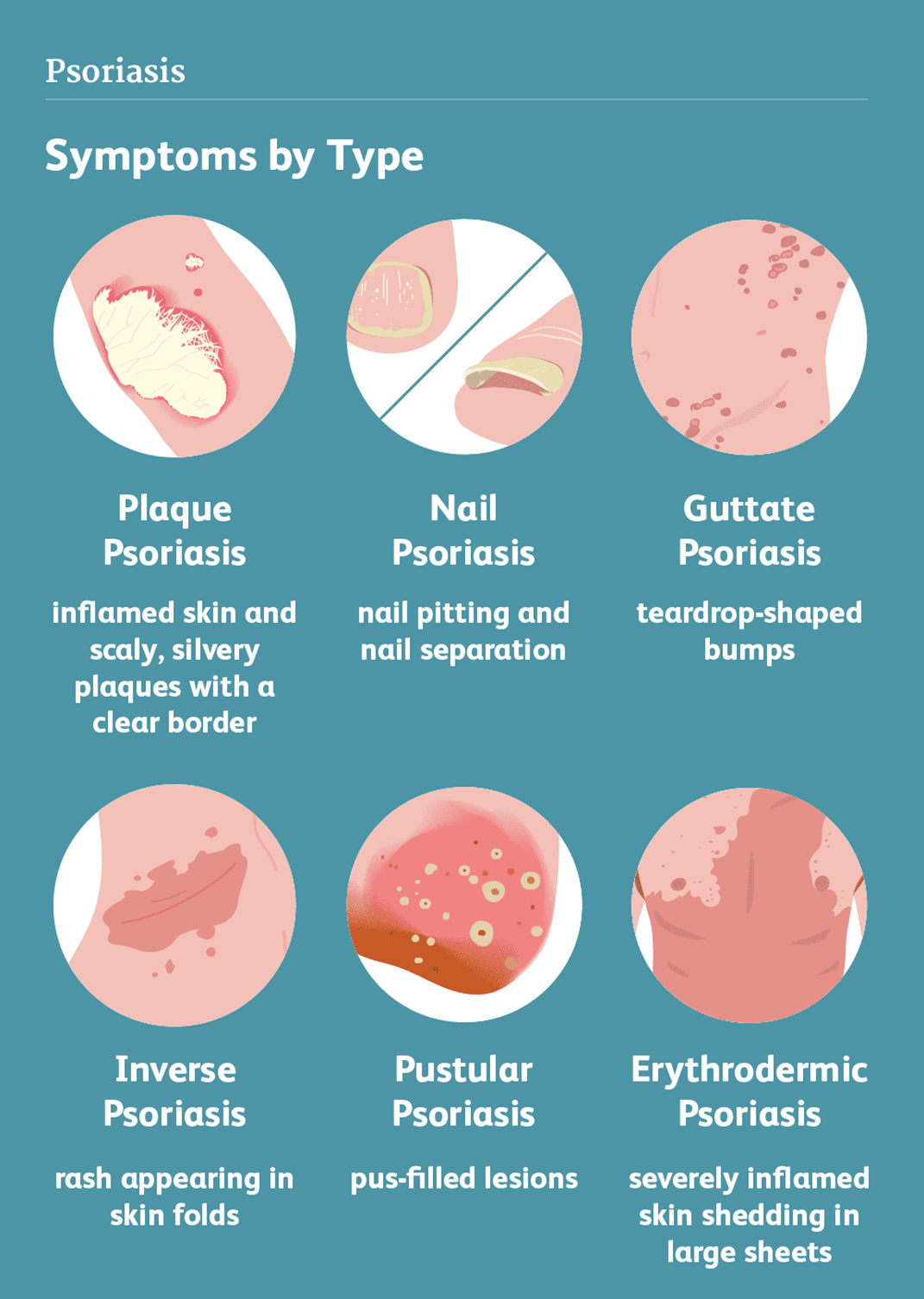
Choice A reason: Psoriasis is a skin abnormality that causes patches of thick, red skin with silvery scales, usually on the elbows, knees, scalp, lower back, or genitals. Psoriasis is a chronic, inflammatory, autoimmune condition that affects the life cycle of skin cells, causing them to build up rapidly on the surface of the skin. Psoriasis can cause itching, burning, pain, or bleeding.
Choice B reason: Rosacea is a skin abnormality that causes redness, flushing, swelling, or pimples, usually on the face, especially the cheeks, nose, chin, or forehead. Rosacea is a chronic, inflammatory, vascular condition that affects the blood vessels and sebaceous glands of the skin. Rosacea can cause sensitivity, stinging, or dryness.
Choice C reason: Scabies is a skin abnormality that causes small, red bumps, blisters, or burrows, usually on the hands, wrists, feet, ankles, or genitals. Scabies is a contagious, parasitic infection that is caused by tiny mites that burrow into the skin and lay eggs. Scabies can cause intense itching, especially at night.
Choice D reason: Stasis dermatitis is a skin abnormality that causes swelling, redness, scaling, or ulcers, usually on the lower legs or ankles. Stasis dermatitis is a chronic, inflammatory condition that results from poor blood circulation in the veins of the legs, causing fluid to leak into the surrounding tissues. Stasis dermatitis can cause pain, itching, or infection.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Choice A reason: Removing the nursing diagnosis in the plan of care since it has not occurred is not a good action, because it does not account for the possibility of future impairment. The client is still at risk for impaired skin integrity due to the prolonged bed rest, and the nurse should continue to monitor and prevent any skin breakdown.
Choice B reason: Keeping the nursing diagnosis in the plan of care the same since the risk factors are still present is the best action, because it reflects the current situation and the potential problem. The client has not developed impaired skin integrity, but the risk factors have not changed. The nurse should maintain the interventions that have been effective in preventing skin impairment, such as turning, repositioning, moisturizing, and inspecting the skin.
Choice C reason: Modifying the nursing diagnosis in the plan of care to impaired skin integrity is not a good action, because it does not match the data. The client has not shown any signs of impaired skin integrity, such as redness, blanching, breakdown, or ulceration. The nurse should not change the diagnosis based on assumptions or predictions, but on evidence.
Choice D reason: Changing the nursing diagnosis in the plan of care to impaired mobility is not a good action, because it does not address the original problem. The client may have impaired mobility due to the bed rest, but that is not the focus of the question. The question is about the risk for impaired skin integrity, which is a different issue that requires different interventions. The nurse should not ignore or replace the existing diagnosis without justification.
Correct Answer is B
Explanation
Choice A reason: "You should never go around people after your baby is born." is not a good response, because it is unrealistic, rigid, and dismissive of the mother's concern. It does not acknowledge the benefits of social interaction and support for the mother and the baby, nor the risks of isolation and depression. It also does not provide any evidence or rationale for the advice.
Choice B reason: "Tell me more about that." is the best response, because it is openended, empathetic, and respectful of the mother's concern. It invites the mother to share her feelings and thoughts, and allows the nurse to explore the source and extent of the mother's anxiety. It also creates an opportunity for the nurse to provide education and reassurance based on the mother's needs.
Choice C reason: "I did that, and my kids turned out just fine." is not a good response, because it is personal, irrelevant, and unprofessional. It does not address the mother's concern, but rather shifts the focus to the nurse's own experience, which may not be applicable or helpful to the mother. It also implies that the mother's concern is unfounded or exaggerated, and may make the mother feel judged or defensive.
Choice D reason: "Why do you think that is a bad idea?" is not a good response, because it is closedended, confrontational, and accusatory. It does not show empathy or respect for the mother's concern, but rather challenges or criticizes it. It may make the mother feel defensive or guilty, and may discourage further communication.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
