The nurse is assessing a client who reports a 3 day history of vomiting and diarrhea and experiencing difficulty in tolerating oral fluids. Which urine specific gravity value would the nurse expect to see on Initial testing?
Reference Range: Urine Specific Gravity [1.005 to 1.03]
1.035.
1.015.
1.005.
1.025.
1.025.
The Correct Answer is A
A. 1.035:
This specific gravity value indicates highly concentrated urine. In the context of a client experiencing vomiting, diarrhea, and difficulty tolerating oral fluids, such a high specific gravity would be indicative of significant dehydration. Dehydration occurs when the body loses more fluid than it takes in, leading to an imbalance in electrolytes and an increase in urine concentration.
B. 1.015:
This specific gravity value falls within the normal reference range for urine specific gravity. In the context of vomiting, diarrhea, and difficulty tolerating oral fluids, a value within the normal range may be less likely. However, it's important to note that initial testing may not reflect the full extent of dehydration, especially if the client's fluid intake has been severely limited over a short period.
C. 1.005:
This specific gravity value is at the lower end of the normal reference range for urine specific gravity. In a client experiencing significant fluid loss through vomiting and diarrhea, the urine may become more concentrated as the body attempts to conserve water. Therefore, a value of 1.005 would be less likely on initial testing in this context.
D. 1.025:
Similar to Option B, this specific gravity value falls within the normal reference range. While it's possible for a dehydrated individual to have a specific gravity within the normal range, a value of 1.025 may be less likely in the context of significant fluid loss through vomiting and diarrhea. However, it's important to consider that dehydration severity and urine concentration can vary among individuals.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
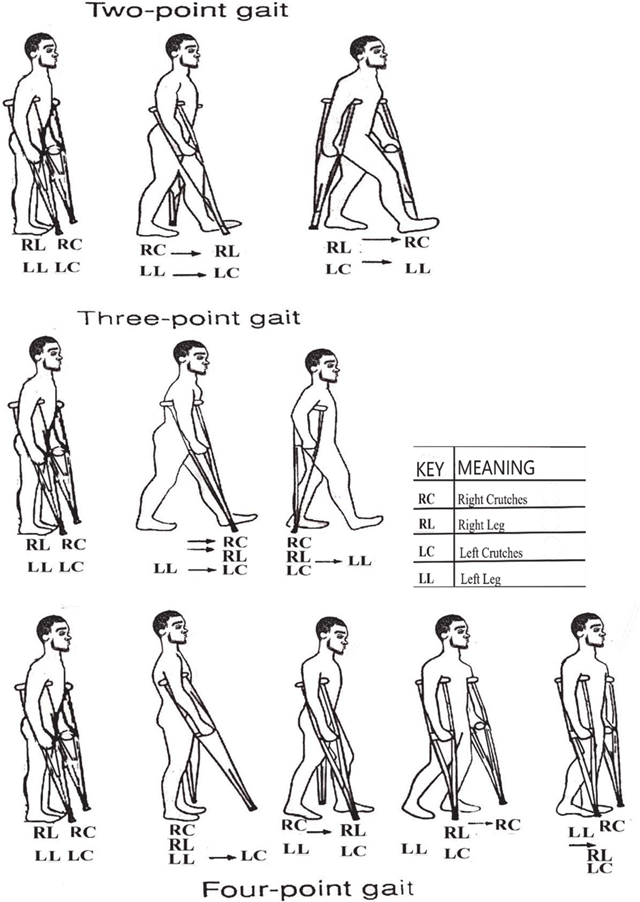
A. Progresses to foot touchdown and weight bearing of affected leg:
This choice indicates that the client understands proper crutch walking because it involves the correct progression of weight-bearing on the affected leg while using the crutches for support. In the three-point gait crutch walking technique, the client progresses by first touching down the foot of the affected leg and then transferring weight onto that leg while stepping forward with the crutches. This behavior ensures proper balance and support during ambulation.
B. Practices bicep and triceps isometric exercises:
This choice does not directly indicate understanding of proper crutch walking. While strengthening the biceps and triceps muscles can be beneficial for overall strength and endurance, it is not a specific behavior related to proper crutch walking technique.
C. Inspects crutches to ensure rubber tips are intact:
While it is important to inspect crutches regularly to ensure they are in good condition, this behavior alone does not necessarily indicate an understanding of proper crutch walking technique. It is more related to equipment maintenance and safety rather than the actual execution of crutch walking.
D. Bears body weight on the palms of hands during the crutch gait:
This choice suggests an incorrect technique. Proper crutch walking technique involves bearing weight on the hands through the hand grips of the crutches rather than the palms. Placing excessive weight on the palms can lead to discomfort, injury, and improper weight distribution, which could hinder effective ambulation.
Correct Answer is C
Explanation
Correct answer: C
A. Irrigate the nasogastric tube with water:
This option is not the best immediate action when a client is choking after vomiting. While irrigating the nasogastric tube with water may help clear the tube itself, it does not directly address the choking episode or potential airway obstruction. The priority in this situation is to ensure the client's airway is clear and maintain their safety.
B. Perform oropharyngeal suctioning:
While suctioning might be used later to clear the airway of secretions, it's not the first-line intervention when someone is actively choking. Suctioning can stimulate the gag reflex and worsen vomiting..
C. Elevate the head of bed 45 degrees:
The primary concern is preventing aspiration (inhaling vomit) which can lead to serious complications. Elevating the head of the bedhelps keep the head and neck in a position that promotes drainage of fluids and reduces the risk of aspiration.
D. Review the advance directive document:
Reviewing the advance directive document is important for understanding the client's wishes regarding their healthcare decisions, but it is not the appropriate action in the immediate management of a choking episode. Ensuring the client's safety and addressing the choking episode take precedence over reviewing documentation.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
