The nurse is planning care for a client diagnosed with SIADH. Which of the following would be included in the plan of care? Select all that apply.
Administer 0.45% NS at 50 mL/hr
Obtain daily weight
Maintain seizure precautions
Administer 3% saline as ordered
Encourage fluid intake
Correct Answer : B,C,D
Choice A Reason:
Administering 0.45% NS (normal saline) at 50 mL/hr is not appropriate for a client with SIADH. This hypotonic solution can exacerbate the condition by increasing the water retention and further diluting the serum sodium levels, worsening hyponatremia. Instead, fluid restriction and hypertonic saline (such as 3% saline) are typically used to manage SIADH.
Choice B Reason:
Obtaining daily weight is crucial in managing SIADH. Daily weights help monitor fluid retention and detect any sudden changes in body weight, which can indicate worsening fluid overload or effective treatment. Accurate weight measurements are essential for assessing the client’s fluid balance and guiding treatment decisions.
Choice C Reason:
Maintaining seizure precautions is necessary for clients with SIADH because severe hyponatremia can lead to neurological symptoms, including seizures. Implementing seizure precautions helps ensure the client’s safety and allows for prompt intervention if a seizure occurs.
Choice D Reason:
Administering 3% saline as ordered is appropriate for treating severe hyponatremia in SIADH. Hypertonic saline helps increase serum sodium levels and reduce the risk of neurological complications. It must be administered carefully and under close monitoring to avoid rapid correction of sodium levels, which can lead to osmotic demyelination syndrome.
Choice E Reason:
Encouraging fluid intake is not appropriate for clients with SIADH. Fluid restriction is a key component of managing SIADH to prevent further dilution of serum sodium levels. Encouraging fluid intake would counteract this goal and worsen the client’s condition.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A Reason:
Telling his wife what the client needs is not the most effective discharge action. While it is important for the wife to understand the client’s needs, this approach is too passive and does not actively engage the client or his wife in the care process. Effective management of Parkinson’s disease requires active participation from both the client and the caregiver to ensure adherence to the care plan and to address any concerns or preferences they may have.
Choice B Reason:
Setting up visitations by a home health nurse can be beneficial, but it is not the most effective discharge action on its own. Home health nurses can provide valuable support and monitoring, but the success of the management plan also depends on the involvement and commitment of the client and his wife. Without their active participation, the care plan may not be fully effective.
Choice C Reason:
Involving the client and his wife in developing a plan of care is the most effective discharge action. This approach ensures that both the client and his wife are fully engaged in the care process, understand the management plan, and are more likely to adhere to it. Collaborative care planning allows for the consideration of the client’s and caregiver’s preferences, needs, and concerns, leading to a more personalized and effective care plan. This active involvement can also empower the client and his wife, improving their confidence in managing the disease.
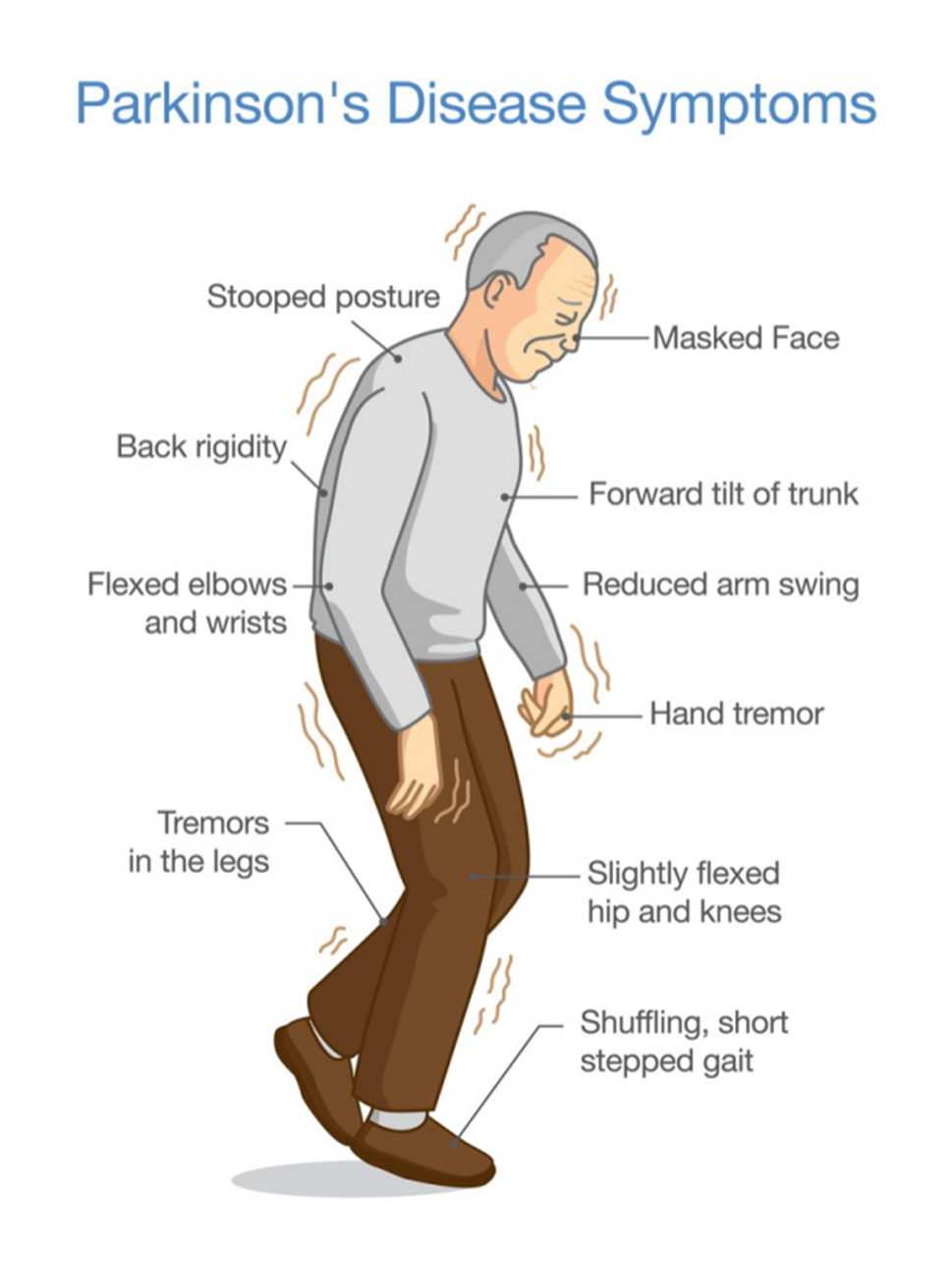
Choice D Reason:
Writing up a detailed plan of care according to standards is important, but it is not the most effective discharge action if done in isolation. A standardized care plan may not address the unique needs and preferences of the client and his wife. Without their involvement in the development of the plan, there may be a lack of understanding or commitment to the care plan, reducing its effectiveness. Personalizing the care plan through active involvement of the client and his wife is crucial for successful management.
Correct Answer is ["C","E"]
Explanation
Choice A: Formed stool in collection pouch
Formed stool in the collection pouch is not expected in an ileostomy. The output from an ileostomy is typically liquid to semi-liquid because the ileum does not absorb as much water as the colon. If formed stool is present, it may indicate a blockage or other issue that needs to be addressed.
Choice B: Stoma is edematous and bleeding
An edematous and bleeding stoma is not a normal finding and may indicate complications such as infection, trauma, or poor stoma care. The stoma should be moist and pink, but not swollen or bleeding. Persistent bleeding or significant edema should be reported to a healthcare provider immediately.
Choice C: Stoma is pink and shiny
A pink and shiny stoma is a sign that the ileostomy is functioning well. This indicates good blood flow and healthy tissue. The stoma should always appear moist and pink, similar to the inside of the mouth. Any deviation from this appearance, such as a pale, dark, or dry stoma, should be evaluated by a healthcare professional.
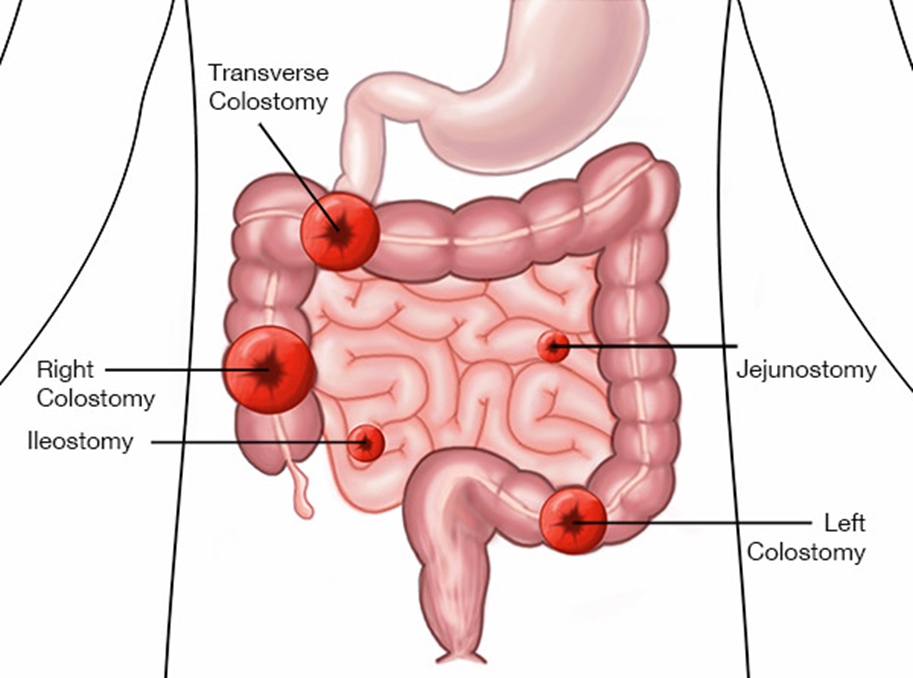
Choice D: Skin excoriation around the stoma
Skin excoriation around the stoma is not a normal finding and suggests that the skin is being irritated by the stoma output or the ostomy appliance. Proper skin care and fitting of the ostomy appliance are essential to prevent skin breakdown. If excoriation occurs, it should be treated promptly to prevent further complications.
Choice E: Mucus liquid flows from the stoma
Mucus liquid flowing from the stoma is expected in an ileostomy. The output is typically liquid to semi-liquid and may contain mucus, which is normal for the small intestine. This type of output indicates that the ileostomy is functioning as intended.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
