The nurse is providing care for a client who has syndrome of inappropriate antidiuretic hormone (SIADH) and is critically ill. Which of the following lab findings requires immediate intervention?
Serum potassium 5.0 mEq/L
Serum calcium 8.0 mg/dL
Serum sodium 125 mEq/L
Blood urea nitrogen (BUN) 24 mg/dL
The Correct Answer is C
Choice A reason:
A serum potassium level of 5.0 mEq/L is within the normal range (3.5-5.0 mEq/L). While it is on the higher end of normal, it does not require immediate intervention in the context of SIADH. Potassium levels are crucial for cardiac and muscle function, but this value does not indicate a critical imbalance.
Choice B reason:
A serum calcium level of 8.0 mg/dL is slightly below the normal range (8.5-10.2 mg/dL). Mild hypocalcemia can occur in various conditions, but it is not typically associated with SIADH and does not require immediate intervention unless symptomatic or significantly lower.
Choice C reason:
A serum sodium level of 125 mEq/L indicates hyponatremia, which is a hallmark of SIADH. Hyponatremia can lead to severe neurological symptoms, including seizures, confusion, and coma, especially if it develops rapidly. Immediate intervention is required to correct the sodium imbalance and prevent serious complications.
Choice D reason:
A blood urea nitrogen (BUN) level of 24 mg/dL is within the upper normal range (7-20 mg/dL). While slightly elevated, it is not critically high and does not require immediate intervention in the context of SIADH. BUN levels can be influenced by various factors, including hydration status and renal function.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
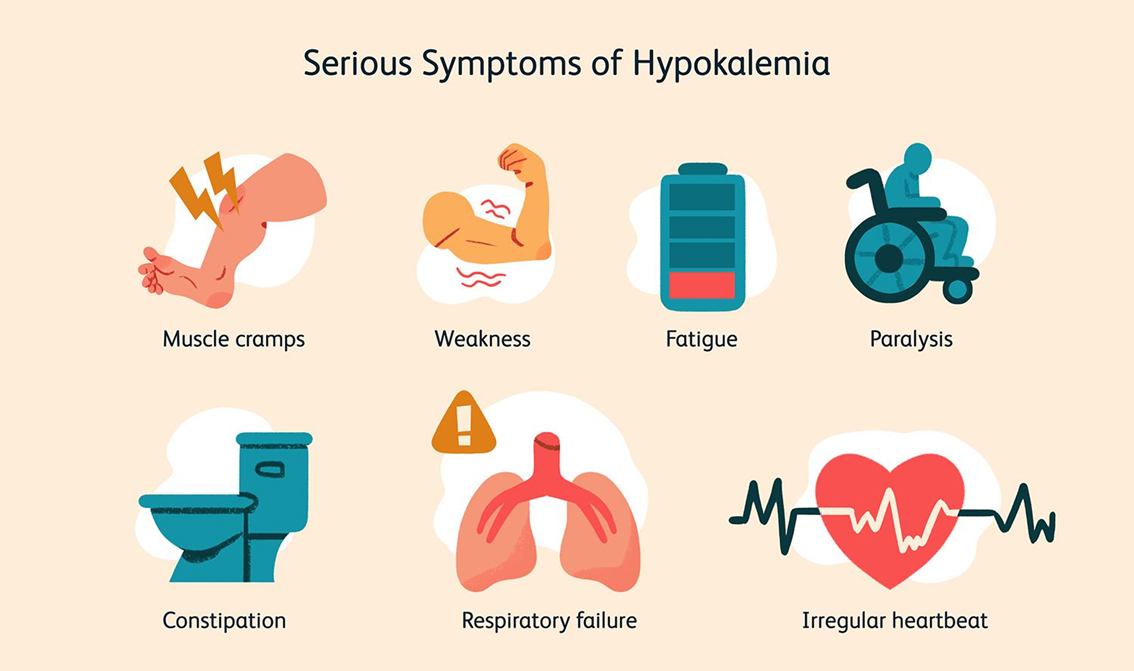
Choice A reason: Hypertension is not directly caused by hypokalemia. While potassium levels can influence blood pressure, hypokalemia is more critically associated with cardiac issues rather than hypertension alone.
Choice B reason: Ketosis is a metabolic state resulting from the body burning fat for fuel instead of carbohydrates. It is not directly related to hypokalemia. Hypokalemia does not cause ketosis, and monitoring for ketosis in a client with hypokalemia is not a priority.
Choice C reason: Insulin resistance is a condition where the body’s cells do not respond properly to insulin. While potassium levels can affect insulin secretion and action, hypokalemia is not primarily associated with insulin resistance. Therefore, it is not the main concern for a nurse monitoring a client with hypokalemia.
Choice D reason: Cardiac arrhythmias are a significant concern in clients with hypokalemia. Potassium is crucial for proper cardiac function, and low levels can lead to abnormal heart rhythms. This is why monitoring for cardiac arrhythmias is essential in clients with hypokalemia.
Correct Answer is C
Explanation
Choice A reason:
A serum potassium level of 5.0 mEq/L is within the normal range (3.5-5.0 mEq/L). While it is on the higher end of normal, it does not require immediate intervention in the context of SIADH. Potassium levels are crucial for cardiac and muscle function, but this value does not indicate a critical imbalance.
Choice B reason:
A serum calcium level of 8.0 mg/dL is slightly below the normal range (8.5-10.2 mg/dL). Mild hypocalcemia can occur in various conditions, but it is not typically associated with SIADH and does not require immediate intervention unless symptomatic or significantly lower.
Choice C reason:
A serum sodium level of 125 mEq/L indicates hyponatremia, which is a hallmark of SIADH. Hyponatremia can lead to severe neurological symptoms, including seizures, confusion, and coma, especially if it develops rapidly. Immediate intervention is required to correct the sodium imbalance and prevent serious complications.
Choice D reason:
A blood urea nitrogen (BUN) level of 24 mg/dL is within the upper normal range (7-20 mg/dL). While slightly elevated, it is not critically high and does not require immediate intervention in the context of SIADH. BUN levels can be influenced by various factors, including hydration status and renal function.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
