The nurse needs to estimate quickly the heart rate of a patient with a regular heart rhythm. Which method will be best to use?
Print a 1-minute electrocardiogram (ECG) strip and count the number of QRS complexes.
Calculate the number of small squares between one QRS complex and the next and divide it into 1500.
Use the 3-second markers to count the number of QRS complexes in 6 seconds and multiply by 10.
Count the number of large squares in the R-R interval and divide by 300.
The Correct Answer is C
This method, known as the 6-second method, involves counting the number of QRS complexes in a 6-second interval on the electrocardiogram (ECG) strip and then multiplying that number by 10 to calculate the heart rate per minute. The advantage of this method is that it provides a relatively quick estimate of the heart rate.
A. Printing a 1-minute ECG strip and counting the number of QRS complexes in (option A) is incorrect because it can be time-consuming and may not be practical in situations where a quick estimate is needed.
B. Calculating the number of small squares between one QRS complex and the next and dividing into 1500 in (option B) is incorrect because it is a method used to calculate heart rate, known as the "1500 method," but it is not as quick as the 6-second method and requires more time and measurement precision.
D. Counting the number of large squares in the R-R interval and dividing by 300 is another method used to calculate heart rate, known as the "300 method," but it is also less quick and less accurate for assessing heart rate in patients with regular rhythms.
It's important to note that if the heart rhythm is irregular, these methods may not provide an accurate estimate of the heart rate, and a longer monitoring period or a different approach may be necessary.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
When the low-pressure alarm sounds, it indicates that the pressure being detected by the arterial line is below the set threshold. This could be due to a variety of reasons, such as a loose connection, air bubbles, or a shift in the zero-reference point.
Rezeroing the monitoring equipment involves recalibrating or resetting the baseline reference point for the arterial pressure waveform. This ensures accurate measurement and monitoring of the patient's arterial pressure.
A. Checking the right hand for a rash in (option A) is incorrect because While assessing the patient for any skin changes or rashes is important, it is not the first action to take in response to a low-pressure alarm.
B. Assessing the waveform for under-dampening in (option B) is incorrect because Assessing the waveform characteristics is important in arterial line monitoring, but it may not be the initial action when the low-pressure alarm sounds. Rezeroing the equipment should be performed before assessing waveform characteristics.
C. Assessing for cardiac dysrhythmias in (option C) is incorrect because Assessing for dysrhythmias is an important aspect of patient care, but it may not be directly related to the low-pressure alarm from the arterial line. Rezeroing the monitoring equipment takes precedence.
Therefore, when the low-pressure alarm sounds for a patient with an arterial line, the nurse should first re-zero the monitoring equipment to ensure accurate measurement of arterial pressure.
Correct Answer is D
Explanation
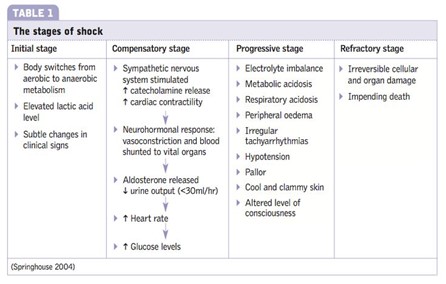
In the compensatory stage of shock, the body initiates various mechanisms to maintain perfusion to vital organs and restore homeostasis. Activation of the renin-angiotensin system is one of the compensatory responses. The decreased blood flow and oxygen delivery to the kidneys stimulate the release of renin from the kidneys. Renin acts on angiotensinogen, converting it into angiotensin I, which is further converted to angiotensin II by the action of angiotensin-converting enzyme (ACE). Angiotensin II is a potent vasoconstrictor and also stimulates the release of aldosterone, leading to sodium and water retention. These mechanisms aim to increase blood pressure and cardiac output and restore fluid balance.
A. The initial stage of shock in (option A) is incorrect because it is characterized by inadequate tissue perfusion and the activation of various compensatory mechanisms, including the release of stress hormones. However, the renin-angiotensin system is not specifically mentioned as activated in this stage.
B. The progressive stage of shock in (option B) is incorrect because it occurs when compensatory mechanisms fail to maintain adequate perfusion, leading to worsening hypoperfusion and organ dysfunction. The renin-angiotensin system continues to be activated during this stage, but it is primarily associated with the compensatory stage.
C. The refractory stage of shock in (option C) is incorrect because it is the stage of severe and prolonged hypoperfusion, where organ failure becomes irreversible. The renin-angiotensin system may still be activated, but it is not the primary focus of this stage.
Therefore, the activation of the renin-angiotensin system occurs during the compensatory stage of shock.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
