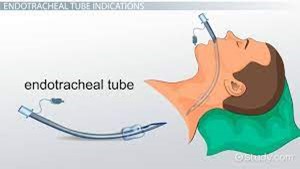
To verify the correct placement of an endotracheal tube (ET) after insertion, the best initial action by the nurse is to:
auscultate for the presence of bilateral breath sounds.
Use an end-tidal C02 monitor to check for placement in the trachea.
Observe the chest for symmetrical movement with ventilation.
Obtain a portable chest radiograph to check tube placement.
The Correct Answer is C
The nurse should listen over both lung fields to ensure that air entry is present bilaterally, indicating that the tube is correctly positioned in the trachea. This comes after observing chest movements.
B. Using an end-tidal CO2 monitor to check for placement in the trachea in (option B) is incorrect because End-tidal CO2 monitoring can provide confirmation of correct tube placement in the trachea by detecting exhaled CO2 levels. However, it requires additional equipment and setup, which may not be readily available at the bedside or immediately accessible.
C. Observing the chest for symmetrical movement with ventilation is the initial action after placing an endotracheal tube.
D. Obtaining a portable chest radiograph to check tube placement (option D) is incorrect because Chest radiographs are commonly used to confirm endotracheal tube placement, especially for long-term confirmation or if there are concerns about placement. However, obtaining a portable chest radiograph may involve delays and is not the initial action to be taken for immediate verification.
Therefore, the best initial action by the nurse to verify the correct placement of an endotracheal tube (ET) after insertion is to auscultate for the presence of bilateral breath sounds.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
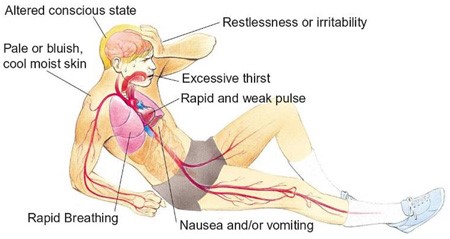
Correct Answer is B
Explanation
Cool, clammy skin, tachycardia, and hypotension are signs of shock, indicating inadequate tissue perfusion and oxygenation. The immediate priority is to ensure adequate oxygen delivery to the tissues. Providing oxygen at 100% via a non-rebreather mask helps increase the patient's oxygen saturation and improve tissue oxygenation.
While all the options mentioned are important in the management of a patient in shock, oxygenation takes priority as it directly addresses compromised tissue perfusion and oxygenation.
A. Inserting two large-bore IV catheters in (option A) is incorrect because: Establishing intravenous access is crucial for fluid resuscitation and administration of medications, but it can be done after ensuring adequate oxygenation.
C. Drawing blood to type and crossmatch for transfusions in (option C) is incorrect because Blood typing and crossmatching are important for potential blood transfusions but should not be the first action in this critical situation.
D. Initiating continuous electrocardiogram (ECG) monitoring in (option D) is incorrect because Continuous ECG monitoring is important for assessing cardiac rhythm and detecting any dysrhythmias, but ensuring oxygenation should be the initial priority.
Therefore, in a patient presenting with cool, clammy skin, tachycardia, and hypotension, the nurse should first provide oxygen at 100% via a non-rebreather mask to address inadequate tissue perfusion and oxygenation.
Correct Answer is C
Explanation
Hypovolemic shock is a life-threatening condition resulting from severe blood or fluid loss. The patient in this scenario exhibits signs of hypovolemic shock, such as low blood pressure, tachycardia, cool and clammy skin, and decreased urine output.
When assessing the prescription options, the nurse should consider the appropriateness of each intervention for hypovolemic shock. Plasmanate is a type of plasma protein fraction that is used for volume expansion in certain situations. However, in hypovolemic shock, the primary intervention is to restore intravascular volume promptly. Plasmanate alone may not be sufficient for rapid-volume resuscitation.
In hypovolemic shock, the initial management typically involves the administration of crystalloid solutions, such as Lactated Ringers or Normal Saline, to restore intravascular volume. Therefore, the prescription of Plasmanate as the primary intervention raises concerns and should be questioned by the nurse.
A. Dopamine (Intropin) 12 mcg/min in (option A) is incorrect because: Dopamine is a vasopressor medication used to increase blood pressure and cardiac output. It is a suitable option for hypovolemic shock to support blood pressure and tissue perfusion.
B. Dobutamine (Dobutrex) 5 mcg/kg/min in (option B) is incorrect because: Dobutamine is an inotropic medication that helps improve cardiac contractility and cardiac output. It can be beneficial in cases of hypovolemic shock with signs of poor cardiac function.
D. Bumetanide (Bumex) 1 mg IV in (option D) is incorrect because: Bumetanide is a loop diuretic used to promote diuresis. However, in the context of hypovolemic shock, diuretics are generally not the first-line treatment as they can further reduce intravascular volume and worsen the patient's condition.
It is essential for the nurse to consult with the healthcare provider regarding the prescription order of Plasmanate and consider alternative interventions for rapid volume resuscitation in hypovolemic shock.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
