What is the most frequently observed side effect of insulin administration?
Hypoglycemia
Anaphylaxis
Nausea
Lipodystrophy
The Correct Answer is A
Choice A rationale:
Hypoglycemia is the most frequent side effect of insulin administration. It occurs when blood glucose levels drop too low, typically below 70 mg/dL.
Insulin is a hormone that plays a key role in regulating blood glucose levels. It works by promoting the uptake of glucose from the bloodstream into cells, where it can be used for energy.
When too much insulin is administered, or when blood glucose levels are already low, it can lead to hypoglycemia. Symptoms of hypoglycemia can vary, but they often include:
Shakiness Sweating Anxiety Hunger Palpitations Confusion Dizziness Blurred vision Seizures
Loss of consciousness
If hypoglycemia is not treated promptly, it can lead to serious complications, such as coma or death.
Therefore, it is important to be aware of the signs and symptoms of hypoglycemia and to take steps to prevent it. This may involve monitoring blood glucose levels regularly, adjusting insulin doses as needed, and carrying a source of fast-acting glucose, such as glucose tablets or juice, to treat hypoglycemia if it occurs.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice A rationale:
Stevens-Johnson syndrome (SJS) is a rare, serious skin condition that is typically caused by an allergic reaction to medication. While amiodarone has been associated with a few cases of SJS, it is not considered a common long-term side effect.
Choice B rationale:
Ventricular tachycardia (VT) is a type of fast heart rhythm that originates in the ventricles of the heart. Amiodarone is actually used to treat VT, so it would be counterintuitive to list it as a long-term side effect.
Choice C rationale:
Pulmonary fibrosis is a condition characterized by scarring of the lung tissue. While amiodarone can cause pulmonary toxicity, which includes pulmonary fibrosis, this is a relatively rare side effect. Moreover, it's usually associated with high doses or
long-term use of the medication.
Choice D rationale:
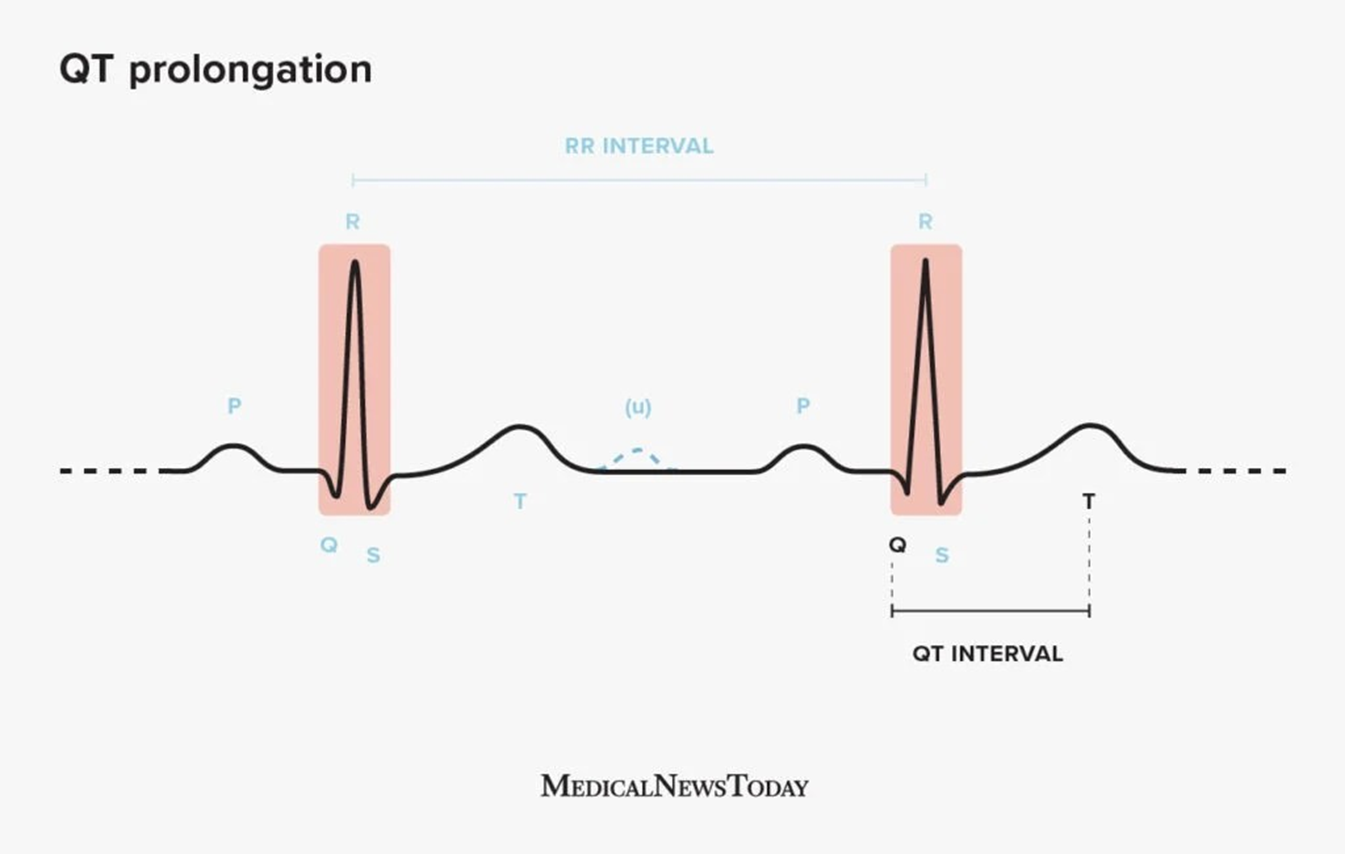
QT prolongation is a condition in which the heart's electrical activity takes longer than normal to recharge between beats. This can lead to a potentially fatal arrhythmia called torsades de pointes. Amiodarone is known to prolong the QT interval, and this is considered one of its most significant long-term side effects. It's important to monitor patients on amiodarone for QT prolongation and to adjust the dose or discontinue the medication if necessary.
Correct Answer is A
Explanation
Choice A rationale:
Hypoglycemia is a critical consideration: The patient's symptoms of lethargy, diaphoresis, and combativeness, along with recent insulin administration, raise a strong suspicion of hypoglycemia (low blood sugar). Hypoglycemia can quickly progress to coma and seizures if not promptly treated, making it a high priority to assess and address.
Bedside glucose testing is rapid and reliable: A bedside finger stick blood glucose test is a quick, non-invasive, and accurate way to determine the patient's blood sugar level. It provides immediate results, allowing for prompt intervention if hypoglycemia is confirmed.
Other assessments and interventions can follow: Once hypoglycemia is ruled out or confirmed, the nurse can proceed with other assessments and interventions as needed.
Choice B rationale:
Insulin administration without blood sugar confirmation is dangerous: Administering insulin without first checking the patient's blood sugar could worsen hypoglycemia if it is already present. This could lead to severe complications, including neurological damage or even death.
Insulin timing is not a priority: While the next dose of insulin may be due, its administration is not the most urgent priority in this situation. Addressing the patient's immediate symptoms and potential hypoglycemia takes precedence.
Choice C rationale:
Naloxone is not indicated for hypoglycemia: Naloxone is an opioid antagonist used to reverse opioid overdose. It has no effect on hypoglycemia and would not be appropriate in this case.
Choice D rationale:
Oxygen therapy may not address the underlying issue: While oxygen therapy can be beneficial for patients with respiratory distress, it does not address the potential hypoglycemia in this case. If the patient's lethargy and combativeness are due to low blood sugar, oxygen therapy alone would not be sufficient treatment.
Oxygen saturation is already within normal limits: The patient's oxygen saturation (SPO2) is 97%, indicating that their oxygenation is currently adequate. Oxygen therapy would not be indicated unless there were signs of hypoxia.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
