The RN is aware that a long-term side effect of amiodarone is:
Stevens-Johnsons Syndrome.
Ventricular Tachycardia.
Pulmonary fibrosis.
QT Prolongation.
The Correct Answer is D
Choice A rationale:
Stevens-Johnson syndrome (SJS) is a rare, serious skin condition that is typically caused by an allergic reaction to medication. While amiodarone has been associated with a few cases of SJS, it is not considered a common long-term side effect.
Choice B rationale:
Ventricular tachycardia (VT) is a type of fast heart rhythm that originates in the ventricles of the heart. Amiodarone is actually used to treat VT, so it would be counterintuitive to list it as a long-term side effect.
Choice C rationale:
Pulmonary fibrosis is a condition characterized by scarring of the lung tissue. While amiodarone can cause pulmonary toxicity, which includes pulmonary fibrosis, this is a relatively rare side effect. Moreover, it's usually associated with high doses or
long-term use of the medication.
Choice D rationale:
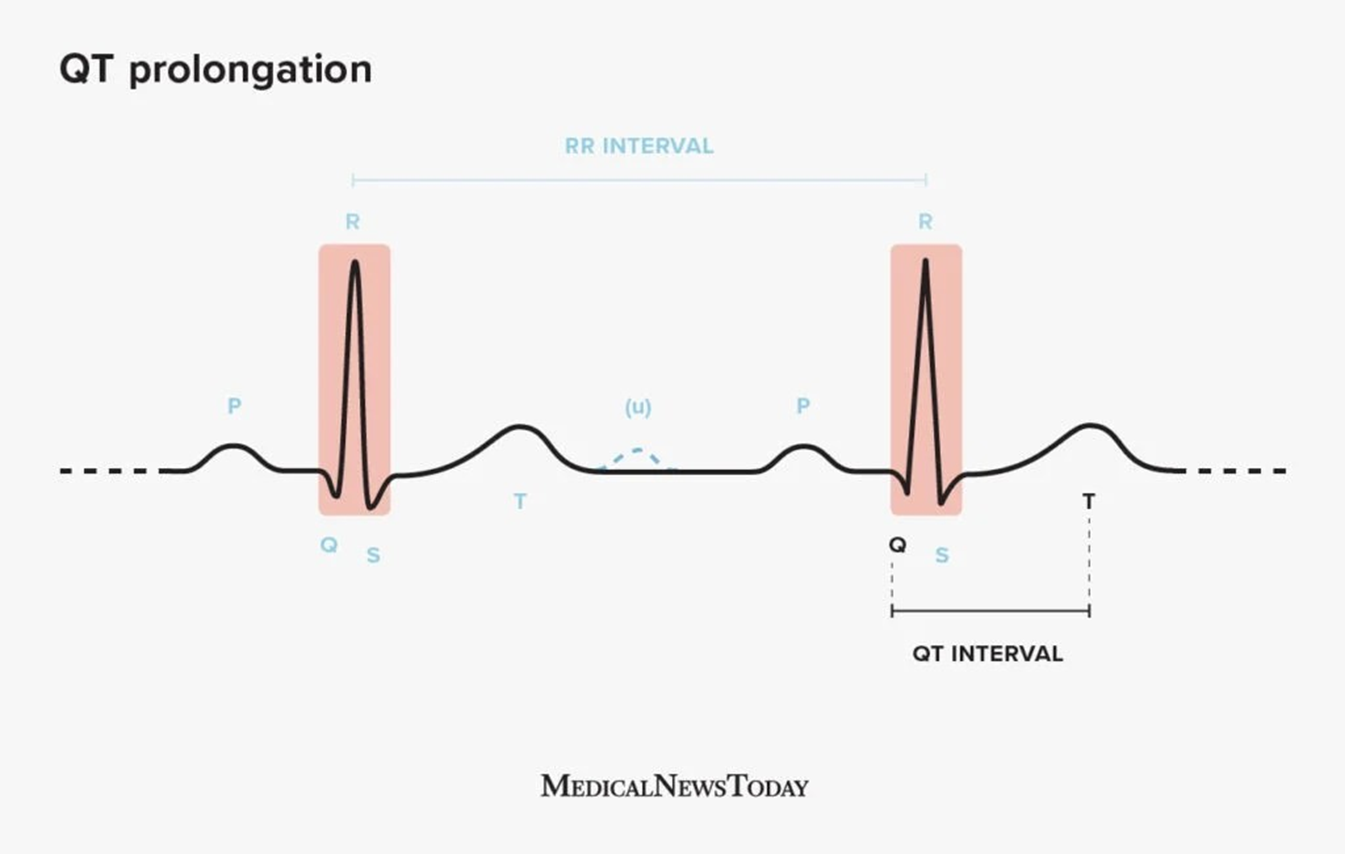
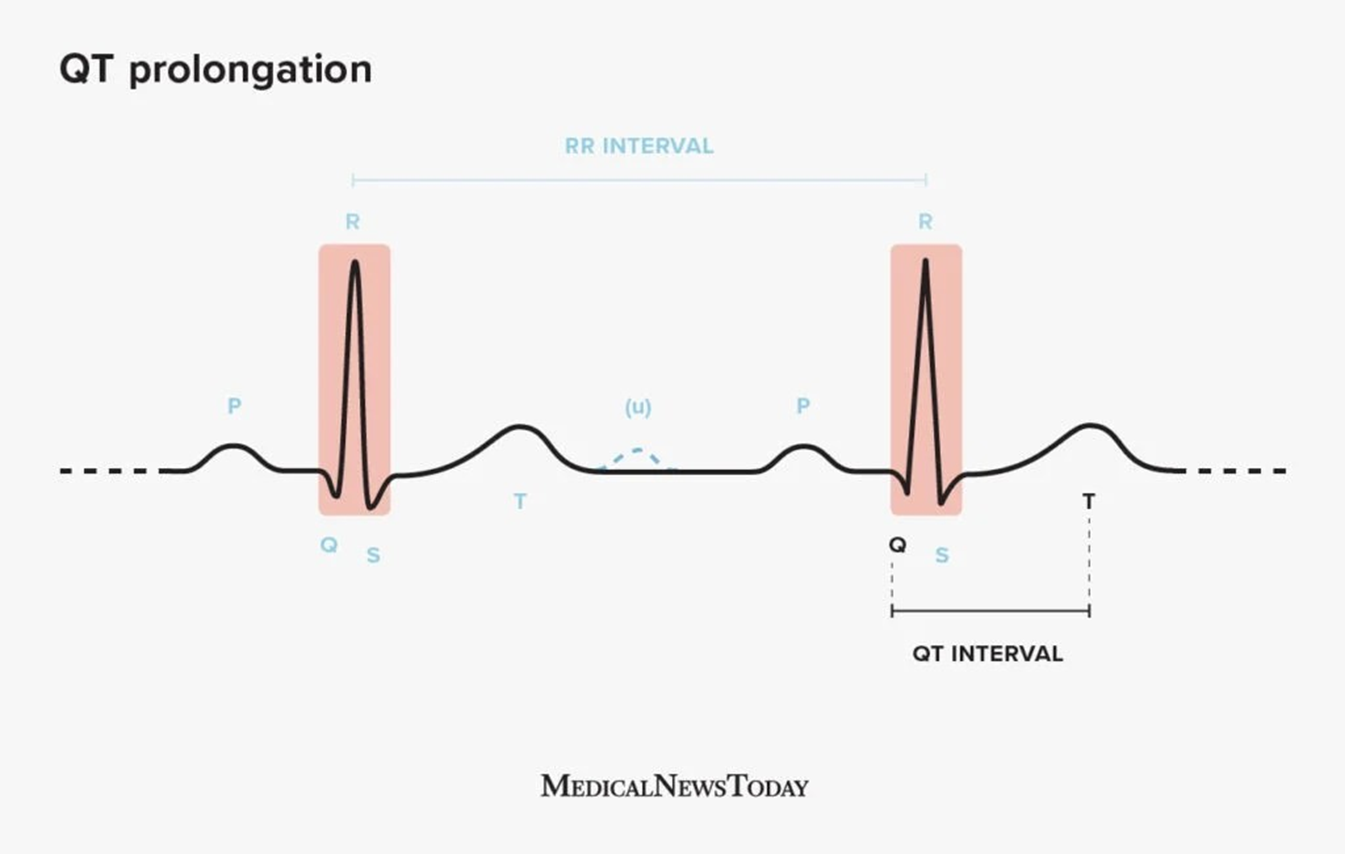
QT prolongation is a condition in which the heart's electrical activity takes longer than normal to recharge between beats. This can lead to a potentially fatal arrhythmia called torsades de pointes. Amiodarone is known to prolong the QT interval, and this is considered one of its most significant long-term side effects. It's important to monitor patients on amiodarone for QT prolongation and to adjust the dose or discontinue the medication if necessary.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Choice A rationale:
Requesting an order for morphine sulfate IV 2 mg over 1-5 minutes would not be appropriate at this time for several reasons: The patient has already received a dose of 4 mg 15 minutes ago, and it has not been effective in relieving the chest pain.
The patient is showing signs of increased respiratory effort, which could be a sign of respiratory depression. Administering an additional dose of morphine could worsen the respiratory depression.
The patient's heart rate is 82 beats per minute, which is within the normal range.
The patient's blood pressure is 135/88 mm Hg, which is also within the normal range.
Choice C rationale:
Administering naloxone (Narcan) to counteract respiratory depression would not be appropriate at this time because the patient is not showing signs of severe respiratory depression. Naloxone is a medication that is used to reverse the effects of opioid overdose. It is typically only used in situations where the patient is experiencing life-threatening respiratory depression.
Choice D rationale:
Administering morphine sulfate IV 4 mg over 1-5 minutes would not be appropriate for the reasons listed above. It could worsen the patient's respiratory depression and potentially lead to other complications.
Choice B is the best answer because it is the most conservative and safest option. By withholding the next dose of morphine and informing the provider about the patient's symptoms, the nurse can ensure that the patient receives the appropriate care and that any potential complications are avoided.
Correct Answer is D
Explanation
Choice A rationale:
Stevens-Johnson syndrome (SJS) is a rare, serious skin condition that is typically caused by an allergic reaction to medication. While amiodarone has been associated with a few cases of SJS, it is not considered a common long-term side effect.
Choice B rationale:
Ventricular tachycardia (VT) is a type of fast heart rhythm that originates in the ventricles of the heart. Amiodarone is actually used to treat VT, so it would be counterintuitive to list it as a long-term side effect.
Choice C rationale:
Pulmonary fibrosis is a condition characterized by scarring of the lung tissue. While amiodarone can cause pulmonary toxicity, which includes pulmonary fibrosis, this is a relatively rare side effect. Moreover, it's usually associated with high doses or
long-term use of the medication.
Choice D rationale:
QT prolongation is a condition in which the heart's electrical activity takes longer than normal to recharge between beats. This can lead to a potentially fatal arrhythmia called torsades de pointes. Amiodarone is known to prolong the QT interval, and this is considered one of its most significant long-term side effects. It's important to monitor patients on amiodarone for QT prolongation and to adjust the dose or discontinue the medication if necessary.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
