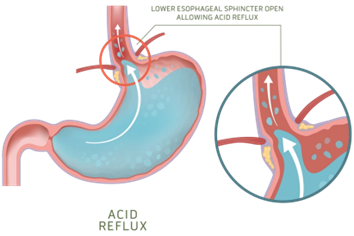
When admitting a patient with a stroke who is unconscious and unresponsive to stimuli. The nurse learns from the patient’s family that the patient has a history of GERD, the nurse will plan to do frequent assessment of the patient’s:
Breath sounds.
abdominal girth.
Bowel sounds.
Apical pulse.
The Correct Answer is A
GERD can increase the risk of aspiration (inhalation of stomach contents into the lungs), which can cause respiratory issues, including abnormal breath sounds. In these cases, monitoring of breath sounds may be more appropriate than monitoring of bowel sounds.
Bowel sounds are not typically monitored for GERD patients as GERD is a condition that affects the esophagus and the stomach, not the intestines. GERD is caused by the reflux of stomach contents into the esophagus, which can cause symptoms such as heartburn and regurgitation.
Abdominal girth is not routinely monitored for GERD patients as it is not typically related to the condition. GERD is a disorder that affects the esophagus and stomach and does not typically cause significant changes in abdominal size or girth. In rare cases, GERD can be complicated by a condition known as a para oesophageal hernia, which can cause a visible bulge in the abdomen. In these cases, monitoring of abdominal size and shape may be necessary.
The apical pulse is not routinely monitored for GERD patients as it is not directly related to the condition. GERD is a disorder that affects the digestive system, specifically the esophagus and stomach and does not typically have an impact on heart rate or rhythm.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
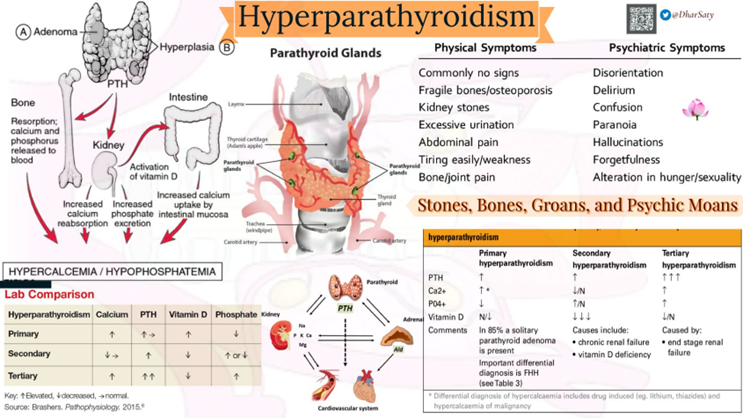
Correct Answer is C
Explanation
The patient with primary hyperparathyroidism has high levels of calcium in the blood (hypercalcemia) which can lead to symptoms such as kidney stones, bone pain, and weakness. High urine calcium levels may also be present due to the increased calcium in the blood.
One important intervention for managing hypercalcemia is to encourage fluid intake to promote increased urine output and prevent the formation of kidney stones. Therefore, the nurse should encourage the patient to drink at least 4000 ml of fluids per day.
Seizure precautions (a), range-of-motion exercises (b), and monitoring for positive Chvostek’s or Trousseaus sign (d) are not directly related to managing hypercalcemia and are not necessary in this case.
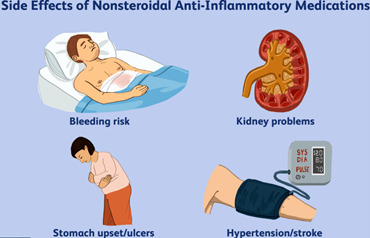
Correct Answer is A
Explanation
NSAIDs are known to be a common cause of acute gastritis. Therefore, it is essential for the nurse to ask the patient about their frequency of NSAID use to determine if this may have caused their current symptoms. Other options such as family history of gastric problems, recent weight gain or loss, and amount of fat in the diet, may also be relevant to the patient's overall health status, but they are not as important as the potential cause of their current condition.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
