Which adverse effect unique to vancomycin is caused by histamine release?
Discoloration of body fluids
Ototoxicity
Red-man syndrome
Nephrotoxicity
The Correct Answer is C
A. Discoloration of body fluids:
Vancomycin can cause discoloration of body fluids, particularly urine, resulting in a brownish discoloration. However, this is not caused by histamine release.
B. Ototoxicity:
Ototoxicity refers to damage to the inner ear structures leading to hearing loss or balance problems. While vancomycin can cause ototoxicity, it is not specifically associated with histamine release.
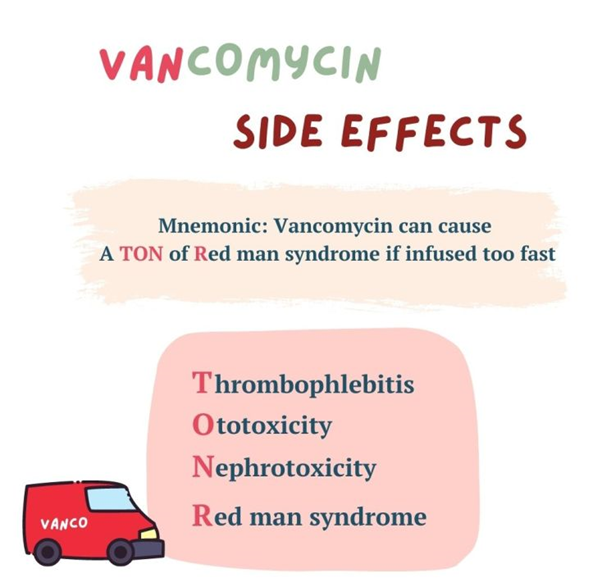
C. Red-man syndrome
Red-man syndrome, also known as red-neck syndrome or red-person syndrome, is a hypersensitivity reaction characterized by flushing of the skin, particularly the upper body and face, resembling a "red man." This reaction is typically associated with the rapid infusion of vancomycin and is caused by the release of histamine from mast cells and basophils. It is not an allergic reaction but rather a non-immunologic response to vancomycin.
D. Nephrotoxicity:
Nephrotoxicity refers to kidney damage caused by certain medications or toxins. While vancomycin can cause nephrotoxicity, it is not specifically associated with histamine release.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["125"]
Explanation
To calculate the rate at which the IV pump should be set to deliver 3,000 mL of intravenous fluids over 24 hours, you would divide the total volume (3,000 mL) by the total time (24 hours):
Rate (mL/hr) = Total volume (mL) / Total time (hours)
Rate = 3,000 mL / 24 hours
Rate ≈ 125 mL/hr
Rounding to the nearest whole number, the IV pump should be set to deliver approximately 125 mL/hr.
Correct Answer is B
Explanation
A. “It’s fine for me to become pregnant while taking this medication.”
This statement is incorrect. Tetracycline is known to have teratogenic effects, meaning it can harm the developing fetus if taken during pregnancy. Women of childbearing age should use effective contraception while taking tetracycline and avoid becoming pregnant during treatment.
B. “I will need to postpone my vacation at the beach until I finish this medication."
This statement demonstrates an understanding of the discharge instructions. Tetracycline can increase the risk of sunburn and photosensitivity reactions. Therefore, it's advisable for the client to avoid prolonged sun exposure, particularly during peak sunlight hours, and to use sun protection measures such as wearing protective clothing, using sunscreen, and avoiding tanning beds or sunlamps. Postponing a vacation at the beach until after finishing the medication is a prudent precaution to minimize the risk of sun-related side effects.
C. “I am so glad to be leaving today because I have an appointment at the tanning salon."
This statement is incorrect. Tetracycline can increase the risk of sunburn and photosensitivity reactions. Visiting a tanning salon while taking tetracycline can further increase the risk of skin damage and should be avoided.
D. "I will stop taking this medication as soon as I feel better.”
This statement is incorrect. It's important for the client to complete the full course of tetracycline as prescribed by their healthcare provider, even if they start to feel better before finishing the medication. Stopping the medication prematurely can lead to incomplete treatment and potential recurrence of the infection.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
