Which vitamin will reduce the therapeutic effects of levodopa?
B6
A
E
K
C
The Correct Answer is A
A. B6 (Pyridoxine):
Vitamin B6, also known as pyridoxine, is known to reduce the therapeutic effects of levodopa. It competes with levodopa for absorption in the gastrointestinal tract and can decrease the amount of levodopa that reaches the brain, thereby diminishing its effectiveness in treating Parkinson's disease symptoms.
B. A (Retinol):
Vitamin A, also known as retinol, is not typically associated with reducing the therapeutic effects of levodopa. Vitamin A plays important roles in vision, immune function, and cellular communication, but it does not interact with levodopa in a way that affects its therapeutic efficacy.
C. E (Alpha-Tocopherol):
Vitamin E, also known as alpha-tocopherol, is an antioxidant that plays a role in protecting cells from oxidative damage. While vitamin E supplementation is sometimes used in Parkinson's disease management for its potential neuroprotective effects, it is not known to reduce the therapeutic effects of levodopa.
D. K (Phylloquinone):
Vitamin K, also known as phylloquinone, is primarily involved in blood clotting and bone metabolism. It does not interact with levodopa in a way that reduces its therapeutic effects.
E. C (Ascorbic Acid):
Vitamin C, also known as ascorbic acid, is not known to reduce the therapeutic effects of levodopa. While vitamin C has various roles in the body, including antioxidant activity and immune function support, it does not interfere with levodopa absorption or efficacy.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["15"]
Explanation
To calculate the dose of amantadine for a client with parkinsonism, the nurse needs to use the following formula:
Dose (mL) = Ordered dose (mg) / Concentration (mg/mL).
In this case, the ordered dose is 150 mg and the concentration is 50 mg/5 mL. Therefore, the dose in mL is:
Dose (mL) = 150 mg / (50 mg/5 mL)
Dose (mL) = 150 mg x (5 mL/50 mg)
Dose (mL) = 15 mL
The nurse should round the answer to the nearest whole number, which is 15 mL. The nurse should administer 15 mL of amantadine oral solution to the client.
Correct Answer is C
Explanation
A. Diarrhea:
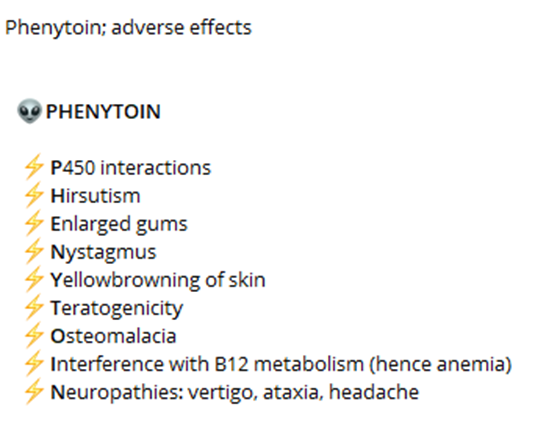
Diarrhea is not a common side effect of phenytoin. While gastrointestinal disturbances such as nausea, vomiting, and constipation may occur, diarrhea is less common. Therefore, it is not a primary adverse effect that the nurse should instruct the client to monitor and report.
B. Wrist pain:
Wrist pain is not a common side effect of phenytoin. Side effects related to musculoskeletal issues such as joint pain, muscle weakness, or muscle twitching can occur, but wrist pain specifically is not commonly associated with phenytoin use. Therefore, it is not a primary adverse effect that the nurse should instruct the client to monitor and report.
C. Skin rash:
Skin rash is a potential adverse effect of phenytoin that should be monitored and reported. Phenytoin can cause various skin reactions, including a mild rash or more severe reactions such as Stevens-Johnson syndrome or toxic epidermal necrolysis. Therefore, the nurse should instruct the client to promptly report any signs of skin rash or other skin changes.
D. Metallic taste:
Metallic taste is a common side effect of phenytoin. While it is not usually a serious adverse effect, it can be bothersome for some individuals. Therefore, the nurse should instruct the client to monitor for this side effect and report it if it occurs persistently or becomes bothersome.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
