Admission and discharge procedures
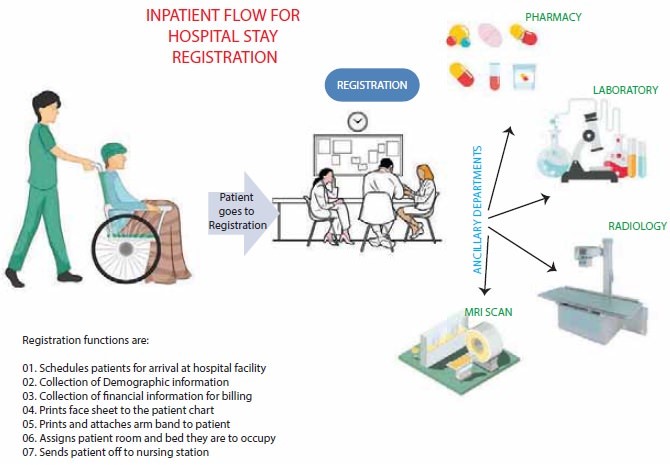
Admission Procedures
The admission process is the first step in establishing a trusting relationship between the nurse, the child, and the family. The nurse should perform the following tasks during admission:
- Verify the child’s identity and assess his or her clinical status.
- Make the child as comfortable as possible and provide appropriate pain relief if needed.
- Introduce the child and family to the staff, roommates, and environment.
- Orient the child and family to the unit policies, routines, facilities, and resources.
- Provide supplies and special equipment needed for daily care, such as diapers, toys, books, games, etc.
- Review the child’s medical history, medication list, allergies, immunizations, growth charts, developmental milestones, etc.
- Obtain baseline vital signs, height, weight, head circumference (for infants), pain score, etc. Normal ranges for vital signs vary by age group. Table 1 shows some examples of normal ranges for different age groups1.
|
Age Group |
Heart Rate (beats/min) |
Respiratory Rate (breaths/min) |
Blood Pressure (mm Hg) |
|
Newborn |
100-160 |
30-60 |
60-90/20-60 |
|
Infant |
100-150 |
25-50 |
70-95/35-65 |
|
Toddler |
90-140 |
20-40 |
80-105/40-70 |
|
Preschooler |
80-110 |
20-30 |
85-110/45-75 |
|
School-age |
75-100 |
15-25 |
90-115/50-80 |
|
Adolescent |
60-90 |
12-20 |
95-120/55-85 |
- Perform a comprehensive physical assessment using a systematic approach. Use developmentally appropriate techniques to elicit cooperation from the child. For example, use distraction, play, or storytelling to reduce anxiety or fear; allow the child to touch or examine equipment before use; explain procedures in simple terms; praise the child for cooperation; etc.
- Collect specimens for laboratory tests as ordered by the physician. Follow standard precautions and infection control measures when handling specimens. Label specimens correctly and transport them to the laboratory promptly.
- Administer medications as ordered by the physician. Follow the six rights of medication administration: right patient, right drug, right dose, right route, right time, right documentation. Use pediatric-specific dosing formulas or charts to calculate drug doses based on the child’s weight or body surface area. Use appropriate devices or techniques to administer medications to children. For example, use oral syringes or droppers for liquid medications; crush tablets or open capsules and mix with food or liquid if allowed; apply topical medications with gloves or cotton swabs; etc.
- Initiate intravenous (IV) therapy as ordered by the physician. Select an appropriate IV site based on the child’s age, condition, and type of infusion. Use an aseptic technique to insert an IV catheter and secure it with tape or dressing. Monitor the IV site for signs of infiltration, phlebitis, infection, or extravasation. Adjust the IV flow rate according to the physician’s order or protocol. Use an infusion pump or controller to deliver accurate and safe IV fluids or medications.
- Implement other interventions as ordered by the physician or indicated by the child’s condition. For example,
- Apply oxygen therapy if the child has hypoxia or respiratory distress. Use an appropriate device to deliver oxygen at the prescribed concentration. Monitor the child’s oxygen saturation level using a pulse oximeter. Assess the child’s respiratory rate, depth, rhythm, effort, breath sounds, etc.
- Insert a nasogastric (NG) tube if the child has vomiting, gastric decompression, feeding intolerance, malnutrition, etc. Use a measuring tape to determine the correct length of insertion based on the child’s nose-to-ear-to-xiphoid process distance. Use a syringe to aspirate gastric contents and check pH level to confirm proper placement. Secure the NG tube with tape or dressing. Monitor the NG tube function, output, patency, etc.
- Insert a urinary catheter if the child has urinary retention, obstruction, infection, incontinence, etc. Use an appropriate size and type of catheter based on the child’s age, gender, and condition. Use an aseptic technique to insert the catheter and collect urine. Secure the catheter with tape or dressing. Monitor the catheter function, output, patency, etc.
- Document all admission data and interventions in the child’s medical record. Use clear, concise, accurate, and timely language. Follow the SOAP format: subjective data (what the child or family says), objective data (what the nurse observes or measures), assessment (what the nurse concludes or diagnoses), and plan (what the nurse plans to do or has done).
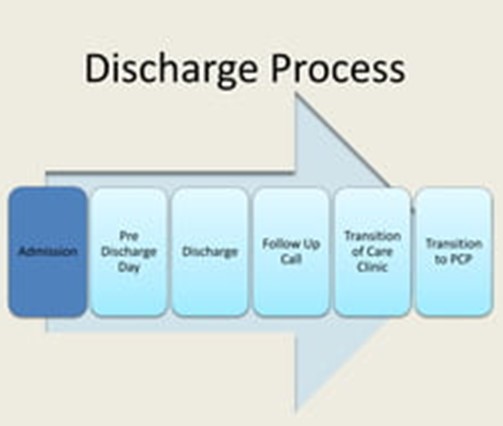
Discharge Procedures
The discharge process is the final step in ensuring a smooth transition from hospital to home for the child and family. The nurse should perform the following tasks during discharge:
- Review the child’s progress and readiness for discharge with the healthcare team. Ensure that the child has met the discharge criteria, such as stable vital signs, adequate pain control, improved symptoms, normal laboratory values, etc.
- Obtain a discharge order from the physician. The order should include the date and time of discharge, the mode of transportation, the destination, and any follow-up instructions or referrals.
- Educate the child and family about the discharge plan and home care. Use developmentally appropriate methods to teach the child and family about the diagnosis, treatment, medications, diet, activity, wound care, infection prevention, signs of complications, when to seek medical attention, etc. Use teach-back or return-demonstration techniques to evaluate the child and family’s understanding and ability to perform home care. Provide written instructions and contact information for questions or concerns.
- Arrange for any necessary equipment, supplies, or services for home care. For example,
- Order a home health nurse or therapist if the child needs skilled care at home.
- Order a durable medical equipment (DME) company to deliver oxygen tanks, infusion pumps, feeding tubes, etc.
- Order a pharmacy to deliver medications or supplies for home use.
- Coordinate with social workers or case managers to arrange for financial assistance, transportation, respite care, etc.
- Reconcile the child’s medications before discharge. Compare the medications that the child was taking before admission with those that he or she will be taking after discharge. Identify any discrepancies or changes and communicate them to the child and family. Provide a complete and accurate list of medications that the child will be taking at home, including names, doses, routes, frequencies, indications, side effects, interactions, etc.
- Perform a final physical assessment and vital signs check on the child. Ensure that the child is stable, comfortable, and ready for discharge. Remove any IV lines, catheters, dressings, etc . that are no longer needed. Apply bandages or ointments as needed. Assist the child with dressing and personal hygiene.
- Collect any valuables or belongings that were stored in the hospital. Return them to the child and family. Check that nothing is left behind in the room.
- Escort the child and family to the exit. Help them with loading their belongings into their vehicle or arranging for transportation. Thank them for choosing your hospital and wish them well.
- Document all discharge data and interventions in the child’s medical record. Use clear, concise, accurate, and timely language. Follow the SOAP format: subjective data (what the child or family says), objective data (what the nurse observes or measures), assessment (what the nurse concludes or diagnoses), and plan (what the nurse plans to do or has done).
Nursing Test Bank
Test Bank #1: RN Pharmacology Exams
Test Bank #2: RN Medical-Surgical Exams
Test Bank #3: RN Fundamentals Exams
Test Bank #4: RN Maternal-Newborn Exams
Test Bank #5: RN Anatomy and Physiology Exams
Test Bank #6: RN Obstetrics and Pediatrics Exams
Test Bank #7: RN Fluid and Electrolytes Exams
Test Bank #9: RN Adult Health
Test Bank #10: RN Dosage Calculation
Test Bank #11: RN Community Health Exams
Test Bank #12: RN Psychology Exams
Test Bank #13: RN Nursing Care Of Children
Test Bank #14: RN Foundations of Nursing Exams
Naxlex Comprehensive Predictor Exams
Exam #1: RN Comprehensive predictor 2023 proctored exam
Exam #2: Ati rn vati comprehensive predictor proctored exam
Exam #3: Ati Rn Comprehensive Predictor Proctored Exam 2023
Exam #4: Rn Comprehensive Predictor 2023 Proctored Exam - St. Joseph
Exam #5: RN Comprehensive Predictor Proctored Exam (National U CA San Diego)
Exam #6: Ati rn comprehensive predictor 2023 retake proctored exam
Exam #7: RN Hesi Exit Proctored Exam
Exam #8: Hesi RN Exit proctored exam
Exam #9: Hesi rn exit proctored exam
Exam #10: Hesi Rn compass exit B proctored exam
Questions on Admission and discharge procedures
Correct Answer is C
Explanation
<p>This instruction is important but not the most important for the nurse to give to the child and family, as it helps identify infection or inflammation of the throat or ears.</p>
Correct Answer is ["A","B","C","D"]
Explanation
<p>This information should be obtained from the child and family, as it helps determine the nutritional status and fluid balance of the child and prepare for surgery if indicated.</p>
Correct Answer is B
Explanation
<p>This statement by the parent indicates a need for further teaching, as it shows a misunderstanding of the pain management instructions. The child should not take aspirin or ibuprofen, as they can increase the risk of bleeding. The child should take acetaminophen or other prescribed medications for pain relief.</p>
Correct Answer is A
Explanation
<p>This action should be taken by the nurse after reviewing the child's immunization record, as it provides important data about the child's risk of allergic reactions or drug interactions.</p>
Correct Answer is B
Explanation
<p>Choice D reason: This statement by the child would indicate that he or she does not understand the discharge instructions, as it may not reflect the wound care or dressing changes after an appendectomy. The child may need to keep the incision site clean and dry, change the bandage as instructed, and report any signs of infection or bleeding.</p>
Correct Answer is C
Explanation
<p>This statement by the child indicates an understanding of the teaching, as it shows awareness of the importance of infection prevention for cystic fibrosis.</p>
Correct Answer is ["A","B","C"]
Explanation
<p>This information is not specific for the discharge plan and home care education for asthma, as it applies to all children regardless of their health condition.</p>
Correct Answer is ["B","C","D"]
Explanation
<p>This information is specific and essential for the nurse to include in the handoff report, as it reflects the secondary problem and intervention for the child who has cystic fibrosis.</p>
<p>Choice D reason: This statement by the nurse may not be appropriate for a 2-year-old toddler, as it does not relate to the physical assessment. It may also distract or confuse the toddler from what is being done.</p>
<p>This action should be taken by the nurse after administering packed red blood cells or platelets as ordered by the physician, as it helps provide information and support to the child and family who may be experiencing fear, anxiety, or grief.</p>
<p>Choice D reason: This is not a good way to obtain the child's cooperation, as it may overwhelm or confuse the child. It also does not involve the child in his or her own care.</p>
No explanation
<p>This instruction is the most important for the nurse to give to the child and family, as it helps prevent sequestration crises, which are episodes of life-threatening organ damage caused by pooling of blood in the spleen or liver due to sickled red blood cells.</p>
<p>This information is important but not the most important for the nurse to communicate during the handoff report. It may be more relevant for the psychosocial assessment and support of the child and family in the ICU.</p>
<p>This statement by the child indicates an understanding of the discharge instructions, as it shows awareness of the signs and symptoms of hyperglycemia, a condition that occurs when the blood sugar level is too high and can lead to diabetic ketoacidosis, a serious complication of diabetes mellitus
<p>This statement by the parent indicates a need for further teaching, as it shows a lack of understanding of the importance of dietary management for diabetes mellitus. The child should follow a balanced and consistent carbohydrate diet that matches the insulin dose and activity level.</p>
Search Here
More on Nursing
Free Nursing Study Materials
Access to all study guides and practice questions for nursing for free.
- Free Nursing Study Trials
- Free Nursing Video tutorials
- Free Nursing Practice Tests
- Free Exam and Study Modes
- Free Nursing Revision Quizlets
