Ati Mental Health Npro 2000 Proctored Exam
Ati Mental Health Npro 2000 Proctored Exam
Total Questions : 41
Showing 10 questions Sign up for moreThe client presents to the emergency department with a headache in the back of the head, diaphoresis, and neck stiffness. The client's blood pressure measures 180/124 mm Hg and heart rate is 168 beats/min. The spouse says the client is currently prescribed "something for depression" and denies any history of cardiac disease. The nurse should suspect the use of what medication?
Explanation
A. MAOIs are a class of antidepressants that work by inhibiting the activity of monoamine oxidase, an enzyme that breaks down neurotransmitters such as serotonin, dopamine, and norepinephrine. MAOIs can interact with certain foods and other medications, potentially leading to a hypertensive crisis characterized by severe hypertension, headache, diaphoresis, and other symptoms.
B. SSRIs are commonly prescribed antidepressants that work by increasing the levels of serotonin in the brain. Serotonin syndrome can present with symptoms such as headache, diaphoresis, tachycardia, and hyperthermia, but it typically doesn't cause severe hypertension.
C. TCAs are another class of antidepressants that work by inhibiting the reuptake of serotonin and norepinephrine. TCAs can cause anticholinergic effects such as dry mouth, blurred vision, constipation, and urinary retention. However, TCAs are less commonly associated with severe hypertension compared to MAOIs.
D. Atypical antipsychotics are used to treat various psychiatric disorders, including schizophrenia and bipolar disorder. While they are not typically associated with causing severe hypertension directly, they can have cardiovascular side effects such as tachycardia and orthostatic hypotension.
A nurse in an acute care mental health facility is caring for a client who has depression. After 3 days of treatment, the nurse notices that the client suddenly seems cheerful and relaxed and there are no longer signs of a depressive state. Which of the following interventions is appropriate to include in the plan of care?
Explanation
A. Sudden change in the client's behavior increases the risk of suicidal behavior and hence requires observation and exploration.
B. Reward the client for her change in behavior: Positive reinforcement can be helpful, but it’s
essential to focus on evidence-based interventions rather than rewards.
C. Open communication is valuable, but it’s essential to approach this conversation with sensitivity. The client may not fully understand the reasons for their sudden change in behavior.
D. Sudden change in the client's behavior increases the risk of suicidal behavior and hence requires observation and exploration. It is therefore, not safe to discharge teh client at this point
A nurse is admitting a client who has experienced a weight loss of 11 kg (25 lb) in the past 3 months. The client weighs 40 kg (88 lb) and believes she is fat. Which of the following aspects of care should the nurse consider the first priority for this client?
Explanation
A. A structured environment can include regular meal times, consistent routines, and clear expectations. While providing a structured environment is important in the overall management of eating disorders, it may not address the immediate concerns related to the client's severe weight loss and distorted body image.
B. Given the client's significant weight loss and distorted body image, assessing their nutritional status is crucial in understanding the extent of the problem and determining appropriateinterventions.
interventions. However, the client’s symptoms point to a mental health problem.
C. While planning a therapeutic diet is an essential component of the client's long-term treatment plan, it may not be the first priority given the client's current medical and psychological status.
D.Given the client's distorted body image, severe weight loss, and belief that she is fat, requesting a mental health consult is not the first priority. The physiological needs should be addressed first
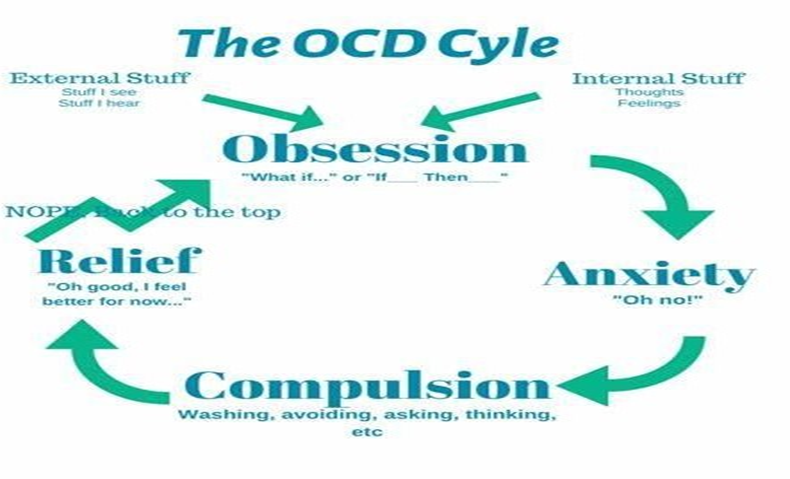
A nurse is caring for a client who has obsessive-compulsive disorder (OCD). Which of the following characteristics are expected findings of OCD? (Select all that apply.)
Explanation
A. In OCD, individuals typically experience intrusive thoughts, images, or urges (obsessions) that cause anxiety or distress, rather than a specific fear of certain objects. While individuals with OCD may engage in compulsive behaviors related to their obsessions.
B. Rule-conscious behavior refers to a strict adherence to rules or regulations. While individuals with OCD may exhibit perfectionist tendencies and a need for orderliness, rule-conscious behavior is not a defining characteristic of OCD.
C. Individuals with OCD may experience difficulty relaxing due to the persistent nature of their obsessions and compulsions. Obsessions can trigger anxiety or distress, making it challenging for individuals with OCD to relax or engage in leisure activities without intrusive thoughts interfering. However, difficulty relaxing is not specific to OCD and can occur in other anxiety disorders as well.
D. Perfectionism is a common feature of OCD. Individuals with OCD often have unrealistic standards for themselves and may engage in compulsive behaviors to achieve a sense of perfection or symmetry. They may feel compelled to repeat tasks until they are "just right" or perform rituals to prevent perceived harm or catastrophe.
E. In OCD, individuals are typically aware of their compulsive behaviors, although they may feel driven to perform them to alleviate anxiety or prevent perceived harm. Compulsions are repetitive behaviors or mental acts that individuals feel driven to perform in response to obsessions or according to rigid rules.
A nurse is providing care to children on a general pediatric unit. Which of the following children should the nurse identify as a potential victim of abuse?
Explanation
B. This behavior may be concerning if it indicates a lack of autonomy or control over one's own communication. It could suggest overprotective or controlling behavior by the parents, which may be indicative of emotional abuse or neglect.
A. Frequent use of the call light may indicate a need for assistance or discomfort but does not necessarily indicate abuse. It could be related to the child's medical condition, anxiety, or other factors.
C. Childhood obesity itself is not necessarily indicative of abuse. It can result from a variety of factors, including genetics, dietary habits, and lifestyle factors.
D. Frequent visitors alone do not necessarily indicate abuse. However, it's important to consider the nature of the visitors' relationship with the child and whether they may pose a risk of harm.
Which behavior would first alert the school nurse or teacher to suspect sexual abuse in a 7-year- old child?
Explanation
C. The child telling sexually explicit stories to peers could be concerning and warrants further investigation. A child speaking in this manner could indicate that they are frequently expose to sexual content of abuse
A. The child has a preference for associating with peers, rather than adults. While this may need further assessment, it does not necessarily point to sexual abuse.
B. Learning problems and shyness alone are not specific indicators of sexual abuse.
D. While poor hygiene and clothing conditions can be signs of neglect, they are not directly related to sexual abuse. Poor hygiene and clothing is more likely to point to child neglect.
A nurse is assessing a client who has schizophrenia and has been on long-term treatment with chlorpromazine. He notes the client is experiencing some involuntary movements of the tongue and face. The nurse should suspect the client has developed which of the following adverse effects?
Explanation
C. Tardive dyskinesia is a movement disorder characterized by repetitive, involuntary movements of the face, tongue, and sometimes other parts of the body. These movements can include lip smacking, tongue protrusion, grimacing, and rapid eye blinking. Tardive dyskinesia is a well-known adverse effect associated with long-term use of antipsychotic medications, particularly first- generation antipsychotics such as chlorpromazine.
A. Neuroleptic Malignant Syndrome is a rare but serious adverse reaction to antipsychotic medications, characterized by symptoms such as severe muscle rigidity, high fever, altered mental status (e.g., confusion), autonomic instability (e.g., fluctuations in blood pressure, heart rate), and elevated creatine phosphokinase (CPK) levels.
B. Dysthymia is a chronic mood disorder characterized by persistent feelings of sadness, hopelessness, and low self-esteem. Dysthymia is not directly related to the involuntary movements described in the scenario and is unlikely to be the cause of the client's symptoms.
D. Akathisia is a movement disorder characterized by inner restlessness and the inability to sit still. Akathisia is a common side effect of antipsychotic medications and can be distressing for affected individuals. However, the symptoms described in the scenario, specifically involuntary movements of the tongue and face, are more indicative of tardive dyskinesia rather than akathisia.
A nurse is caring for a newly admitted client who has obsessive-compulsive disorder (OCD). Which of the following actions should the nurse take first?
Explanation
B. Understanding the precipitating factors is essential for developing effective treatment strategies tailored to the individual's specific needs. By identifying triggers, the nurse can work with the client to develop coping mechanisms and interventions to manage these triggers and reduce the frequency or intensity of obsessive-compulsive symptoms.
A. Providing a structured activity schedule can be helpful for individuals with OCD as it can promote a sense of routine and predictability. However, while structuring activities is beneficial, it may not address the immediate needs of the client upon admission.
C. Teaching relaxation techniques, such as deep breathing exercises, progressive muscle relaxation, or guided imagery, can be beneficial for managing anxiety and stress associated with OCD symptoms. However, like option A, while relaxation techniques are important, they may not address the immediate needs of the client upon admission.
D. Exploring alternative coping strategies with the client involves brainstorming and discussing various techniques or approaches to managing obsessive-compulsive symptoms. However, identification of triggers is a priority.
A nurse is creating a plan of care for a client who is experiencing mania. Which of the following interventions should the nurse include in the plan? (Select all that apply.)
Explanation
A. Providing frequent meals and snacks is generally beneficial, it’s essential to focus on nutritious options.
C. Manic episodes can lead to impulsive behavior, increased activity, and risk-taking. Close monitoring ensures early detection of any safety concerns, such as self-harm or aggression.
D. Manic clients are often hypersensitive to stimuli, and a calm, low-stimulation environment can help reduce agitation and prevent exacerbation of symptoms.
E. While adequate rest is essential, discouraging daytime naps may help regulate the client’s sleep patterns and prevent excessive energy levels associated with mania.
B. Regular weight monitoring is essential for assessing overall health, but it may not be a priority specifically related to mania.
A nurse is caring for an adolescent who is experiencing indications of depression. Which of the following findings should the nurse expect? (Select all that apply.)
Explanation
B. Individuals experiencing depression may have negative thoughts about themselves, feelings of worthlessness, and a diminished sense of self-esteem. These negative self-perceptions can contribute to feelings of hopelessness and despair.
C. Insomnia is a common sleep disturbance associated with depression. Sleep disturbances are prevalent among individuals with depression and can exacerbate other symptoms such as fatigue, irritability, and difficulty concentrating.
D. Individuals with depression may experience irritability, mood swings, and a low tolerance for frustration. Irritability can be a manifestation of the emotional distress and dysregulation often experienced in depression.
A. While some individuals with depression may experience physical symptoms such as headaches and digestive disturbances, these symptoms are not specific to depression
E Euphoria is not a typical finding in depression. Instead, euphoria is more commonly associated with mood disorders such as bipolar disorder
You just viewed 10 questions out of the 41 questions on the Ati Mental Health Npro 2000 Proctored Exam Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



