RN medical surgical hesi Exam
RN medical surgical hesi Exam
Total Questions : 39
Showing 10 questions Sign up for moreA client with acute renal injury (AKI) weighs 110.3 pounds (50 kg) and has a potassium level of 6.7 mEq/L (6.7 mmol/L) is admitted to the hospital. Which prescribed medication should the nurse administer first?
Reference Range:
Potassium [3.5 to 5 mEq/L (3.5 to 5 mmol/L)]
Explanation
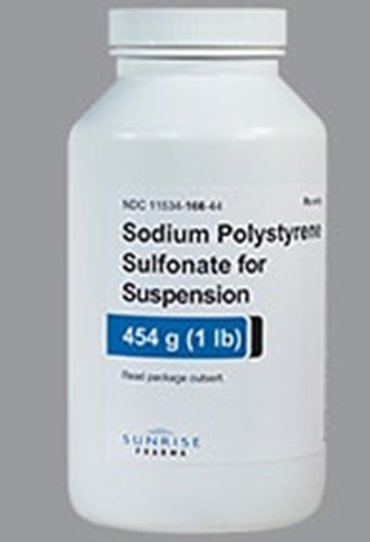
Choice A reason: Sodium polystyrene sulfonate is a medication that binds to excess potassium in the gastrointestinal tract and removes it from the body through feces. It is used to treat hyperkalemia, which is a high level of potassium in the blood. Hyperkalemia can cause cardiac arrhythmias and muscle weakness, and it is a common complication of AKI. Therefore, this medication should be administered first to lower the potassium level and prevent life-threatening complications.
Choice B reason: Sevelamer is a medication that binds to phosphorus in the gastrointestinal tract and removes it from the body through feces. It is used to treat hyperphosphatemia, which is a high level of phosphorus in the blood. Hyperphosphatemia can cause bone loss and soft tissue calcification, and it is a common complication of chronic kidney disease (CKD). However, it is not an urgent issue in AKI, and it does not affect the potassium level.
Choice C reason: Calcium acetate is a medication that also binds to phosphorus in the gastrointestinal tract and removes it from the body through feces. It has the same effect and indication as sevelamer, but it also provides calcium supplementation. However, it is not an urgent issue in AKI, and it does not affect the potassium level.
Choice D reason: Epoetin alfa, recombinant is a medication that stimulates the production of red blood cells in the bone marrow. It is used to treat anemia, which is a low level of hemoglobin or red blood cells in the blood. Anemia can cause fatigue, weakness, and shortness of breath, and it is a common complication of CKD and AKI. However, it is not an urgent issue in AKI, and it does not affect the potassium level.
The nurse is preparing an older client for a magnetic resonance imaging (MRI) with contrast. Which laboratory value should the nurse report to the healthcare provider before the scan is performed?
Reference Range:
Glycosylated hemoglobin (A1C) [4% to 5.9%]
Creatinine [0.5 to 1.1 mg/dL (44 to 97 umol/L)]
Glucose [74 to 106 mg/dL (4.1 to 5.9 mmol/L)]
Blood Urea Nitrogen (BUN) [10 to 20 mg/dL (3.6 to 7.1 mmol/L)]
Explanation
Choice A reason: Fasting blood sugar of 200 mg/dL (11.1 mmol/L) indicates hyperglycemia, which is a high level of glucose in the blood. It can be caused by diabetes mellitus, stress, infection, or medication. Hyperglycemia can cause symptoms such as thirst, hunger, frequent urination, fatigue, and blurred vision. However, it does not affect the safety or accuracy of MRI with contrast.
Choice B reason: Glycosylated hemoglobin A1c of 8% indicates poor glycemic control over the past three months. It can be caused by diabetes mellitus, chronic kidney disease, or hemoglobinopathy. Glycosylated hemoglobin A1c reflects the average blood glucose level over the lifespan of red blood cells, which is about 120 days. However, it does not affect the safety or accuracy of MRI with contrast.
Choice C reason: Blood urea nitrogen of 22 mg/dL (7.9 mmol/L) indicates mild azotemia, which is a high level of nitrogenous waste products in the blood. It can be caused by dehydration, high protein intake, gastrointestinal bleeding, or kidney impairment. Azotemia can cause symptoms such as nausea, vomiting, confusion, and lethargy. However, it does not affect the safety or accuracy of MRI with contrast.
Choice D reason: Serum creatinine of 1.9 mg/dL (169 umol/L) indicates moderate renal insufficiency, which is a reduced ability of the kidneys to filter and excrete waste products and fluids from the body. It can be caused by diabetes mellitus, hypertension, glomerulonephritis, or nephrotoxic drugs. Renal insufficiency can cause symptoms such as edema, anemia, electrolyte imbalance, and acidosis. It can also increase the risk of contrast-induced nephropathy, which is a sudden deterioration of kidney function after exposure to contrast media used for imaging studies such as MRI. Contrast-induced nephropathy can lead to acute kidney injury, dialysis requirement, or even death. Therefore, serum creatinine should be reported to the healthcare provider before MRI with contrast to assess the risk and benefit of the procedure and to take preventive measures such as hydration, medication adjustment, or alternative imaging modalities.
A client with type 1 diabetes mellitus, hypertension, and chronic kidney disease is to begin hemodialysis treatment. Which statement should the nurse include in client education?
Explanation
Choice A reason: An abdominal catheter is used for peritoneal dialysis, not hemodialysis. Hemodialysis requires access to a large blood vessel, usually in the arm or leg.
Choice B reason: Routine medications may need to be adjusted or avoided before or after hemodialysis, depending on their effects on blood pressure, fluid balance, and electrolytes.
Choice C reason: Insulin dosage may need to be reduced during hemodialysis because insulin is removed by the dialyzer and blood glucose levels may drop. This is the correct statement to include in client education.
Choice D reason: Potassium-rich foods should be limited in the diet of clients with chronic kidney disease and hemodialysis, because potassium can build up in the blood and cause cardiac arrhythmias.
A patient is admitted to the hospital with symptoms consistent with a right hemisphere stroke. Which neurovascular assessment requires immediate intervention by the nurse?
Explanation
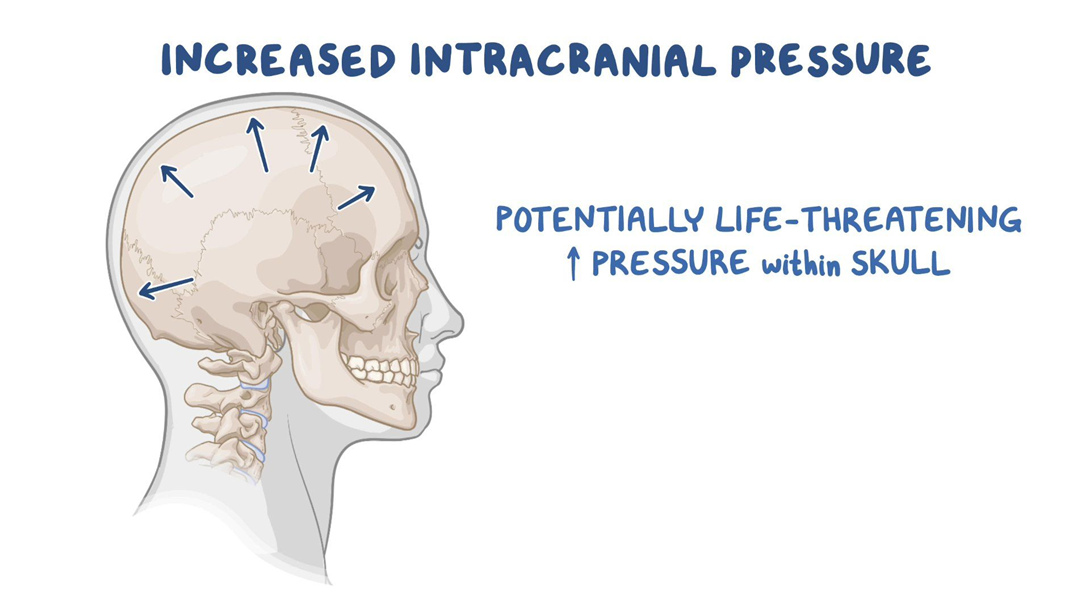
Choice A reason: Pupillary changes to ipsilateral dilation indicate increased intracranial pressure, which is a life-threatening complication of stroke. The nurse should notify the physician and prepare for emergency measures.
Choice B reason: Left-sided facial drooping and dysphagia are common signs of right hemisphere stroke, but they do not require immediate intervention by the nurse. The nurse should monitor the patient's swallowing ability and provide oral care.
Choice C reason: Orientation to person and place only is a sign of impaired cognition, which is also common in right hemisphere stroke. The nurse should assess the patient's memory, judgment, and attention span.
Choice D reason: Unequal bilateral hand grip strengths are a sign of hemiparesis, which is a weakness on one side of the body. The nurse should assist the patient with mobility and prevent contractures.
After performing a head-to-toe assessment for a client with Addison's disease, the nurse reports findings to the healthcare provider. The findings include moist mucous membranes, strong palpable peripheral pulses, and blood pressure 132/88 mm Hg. The client verbalizes understanding of the illness and importance of taking medications every day. Which action should the nurse implement?
Explanation
Choice A reason: A referral for social services at home is not necessary for a client with Addison's disease who has stable vital signs, adequate hydration, and good self-care knowledge.
Choice B reason: Limiting daily fluid intake to 500 mL is not appropriate for a client with Addison's disease, who is at risk of dehydration and hypotension. The client should drink fluids according to thirst and urine output.
Choice C reason: Preparing the client for discharge home is the best action for the nurse to implement, as the client has no signs of complications or deterioration from Addison's disease. The client should be able to manage the condition at home with regular follow-up and medication adherence.
Choice D reason: Strict intake and output monitoring is not required for a client with Addison's disease who has normal blood pressure, moist mucous membranes, and strong peripheral pulses. These indicate adequate fluid balance and renal function.
A client who had a biliopancreatic diversion procedure (BPD) 3 months ago is admitted with severe dehydration. Which assessment finding warrants immediate intervention by the nurse?
Explanation
Choice A reason: Gastroccult positive emesis indicates the presence of blood in the vomit, which is a sign of a serious complication such as anastomotic leak, ulcer, or bleeding. The nurse should notify the physician and monitor the client's vital signs and hemoglobin level.
Choice B reason: Strong foul smelling flatus is a common side effect of BPD, which involves bypassing a large portion of the small intestine and creating a connection between the stomach and the colon. This results in malabsorption and bacterial overgrowth, which produce gas and odor.
Choice C reason: Complaint of poor night vision is a sign of vitamin A deficiency, which can occur after BPD due to reduced absorption of fat-soluble vitamins. The nurse should advise the client to take vitamin supplements and eat foods rich in vitamin A, such as carrots, sweet potatoes, and spinach.
Choice D reason: Loose bowel movements are another common side effect of BPD, which causes diarrhea and steatorrhea (fatty stools). The nurse should encourage the client to drink fluids with electrolytes and avoid foods that worsen diarrhea, such as greasy, spicy, or sugary foods.
A client with a closed head injury demonstrates signs of syndrome of inappropriate antidiuretic hormone (SIADH). Which additional finding should the nurse expect to obtain?
Explanation
Choice A reason: Weight gain of 2 pounds (0.91 kg) in one day is a sign of fluid retention, which occurs in SIADH due to excessive secretion of antidiuretic hormone (ADH). ADH causes the kidneys to reabsorb water and reduce urine output, leading to hyponatremia and hypervolemia.
Choice B reason: Fremitus over the chest wall is a sign of increased vibration or air movement in the lungs, which can indicate pneumonia, bronchitis, or pleural effusion. These are not related to SIADH, but may be complications of head injury or fluid overload.
Choice C reason: Serum sodium of 150 mEq/L (150 mmol/L) is a sign of hypernatremia, which is a high level of sodium in the blood. This is the opposite of what happens in SIADH, where sodium levels are low due to dilution by excess water.
Choice D reason: Urine specific gravity of 1.004 is a sign of diluted urine, which indicates low concentration of solutes in the urine. This is also the opposite of what happens in SIADH, where urine is concentrated and has a high specific gravity.
Following a motor vehicle accident, a client with chest trauma receives a chest tube to relieve a hemothorax. Two hours following the chest tube insertion, the nurse observes the water level in the water-seal chamber is rising during inspiration and falling during expiration. Which action should the nurse implement?
Explanation
Choice A reason: Lifting and clearing drainage from the chest tube is not necessary, as the water level fluctuations indicate that the chest tube is functioning properly and allowing air and fluid to escape from the pleural space.
Choice B reason: Inspecting the tube insertion site for leaking is not indicated, as there is no evidence of air leak in the water-seal chamber. An air leak would cause continuous or intermittent bubbling in the water-seal chamber.
Choice C reason: Continuing to monitor the drainage system is the best action for the nurse to implement, as the water level fluctuations are normal and expected in a water-seal drainage system. The water level should rise during inspiration and fall during expiration, reflecting the changes in intrathoracic pressure.
Choice D reason: Auscultating lungs for unequal breath sounds is not relevant, as it does not address the question of what to do with the water level fluctuations. Unequal breath sounds may indicate a pneumothorax or atelectasis, which are complications of chest trauma or chest tube insertion.

The nurse is caring for a client who had an appendectomy 4 hours ago. Which finding requires immediate action by the nurse?
Explanation
Choice A reason: Redness and edema noted at the incision site are signs of inflammation, which are normal in the early stages of wound healing. The nurse should monitor the site for signs of infection, such as purulent drainage, increased pain, or fever.
Choice B reason: Apical heart rate of 100 to 110 beats/minute is a sign of tachycardia, which may be caused by pain, anxiety, dehydration, or blood loss. The nurse should assess the client's vital signs, fluid status, and hemoglobin level, and administer pain medication as prescribed.
Choice C reason: High-pitched sound heard upon inspiration is a sign of stridor, which is a life-threatening emergency that indicates airway obstruction. The nurse should call for help, administer oxygen, and prepare for intubation or tracheostomy.
Choice D reason: Pain rating of 8 on a scale of 0 to 10 is a sign of severe pain, which may impair the client's recovery and increase the risk of complications. The nurse should administer pain medication as prescribed and use non-pharmacological methods to relieve pain, such as positioning, distraction, or relaxation techniques.
A client who received 6 units of packed red blood cells 3 days ago for a lower gastrointestinal (GI) bleed is now displaying signs of shortness of breath with occasional stridor and is reporting muscle cramping.
Reference Range:
Potassium [3.5 to 5 mEq/L (3.5 to 5 mmol/L)]
Magnesium [Adult: 1.3 to 2.1 mEq/L (0.65 to 1.05 mmol/L)]
Calcium [9 to 10.5 mg/dL (2.3 to 2.6 mmol/L)]
Sodium (136 to 145 mEq/L (136 to 145 mmol/L)]
Which serum laboratory value should the nurse immediately report to the healthcare provider?
Explanation
Choice A reason: Potassium 4.7 mEq/L (4.70 mmol/L) is within the normal reference range of 3.5 to 5 mEq/L (3.5 to 5 mmol/L). Potassium is an electrolyte that helps regulate the balance of fluids and acids in the body, as well as the function of nerves and muscles. A high potassium level (hyperkalemia) can cause muscle weakness, irregular heartbeat, and cardiac arrest. A low potassium level (hypokalemia) can cause muscle cramps, fatigue, and arrhythmias.
Choice B reason: Magnesium 2.1 mEq/L (0.86 mmol/L) is within the normal reference range of 1.3 to 2.1 mEq/L (0.65 to 1.05 mmol/L). Magnesium is an electrolyte that helps regulate the activity of enzymes, muscles, and nerves, as well as the balance of calcium and potassium in the body. A high magnesium level (hypermagnesemia) can cause nausea, vomiting, flushing, muscle weakness, and respiratory depression. A low magnesium level (hypomagnesemia) can cause muscle twitching, tremors, seizures, and cardiac arrhythmias.
Choice C reason: Calcium 6.5 mg/dL (1.63 mmol/L) is below the normal reference range of 9 to 10.5 mg/dL (2.3 to 2.6 mmol/L). Calcium is an electrolyte that helps regulate the function of muscles, nerves, bones, and blood clotting. A high calcium level (hypercalcemia) can cause nausea, vomiting, constipation, confusion, kidney stones, and bone pain. A low calcium level (hypocalcemia) can cause muscle spasms, cramps, tingling, numbness, and stridor (a high-pitched sound when breathing). **This is a critical value that should be immediately reported to the healthcare provider**, as it can indicate a serious condition such as acute pancreatitis, sepsis, or massive blood transfusion.
Choice D reason: Sodium 135 mEq/L (135 mmol/L) is slightly below the normal reference range of 136 to 145 mEq/L (136 to 145 mmol/L). Sodium is an electrolyte that helps regulate the balance of fluids and acids in the body, as well as the function of nerves and muscles. A high sodium level (hypernatremia) can cause thirst, dry mouth, confusion, seizures, and coma. A low sodium level (hyponatremia) can cause headache, nausea, vomiting, fatigue, muscle weakness, and confusion.
You just viewed 10 questions out of the 39 questions on the RN medical surgical hesi Exam Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



