A charge nurse is teaching a newly licensed nurse about Rho(D) immune globulin administration. Which of the following should the charge nurse include as an indication for the administration of Rho(D) immune globulin?
Hyperemesis gravidarum
Rh-positive blood test results
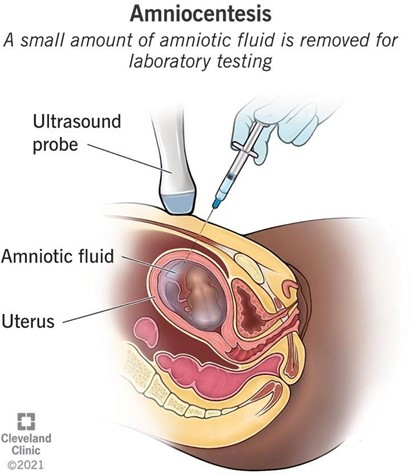
Prescription for an amniocentesis
Anemia
The Correct Answer is C
This is because a prescription for an amniocentesis is an indication for the administration of Rho(D) immune globulin (RhIG) to prevent RhD isoimmunization in mothers who are RhD negative¹². RhD isoimmunization is a condition where the mother's immune system produces antibodies against the RhD antigen on the baby's red blood cells, which can cause hemolytic disease of the newborn (HDN)¹². RhIG is a medication that contains antibodies against the RhD antigen, and it works by binding to and destroying any fetal red blood cells that may enter the maternal circulation, preventing the mother from making her own antibodies¹²³. RhIG is usually given to RhD negative mothers during pregnancy and after delivery if the baby is RhD positive¹².
Amniocentesis is a procedure where a needle is inserted into the uterus to obtain a sample of amniotic fluid, which contains fetal cells and other substances⁴. Amniocentesis can be done for various reasons, such as genetic testing, fetal lung maturity assessment, or infection diagnosis⁴. However, amniocentesis also carries a risk of causing bleeding or leakage of amniotic fluid, which can result in fetal-maternal hemorrhage (FMH), where fetal blood cells enter the maternal circulation⁴⁵. FMH can trigger RhD isoimmunization in RhD negative mothers, so they should receive RhIG within 72 hours of the procedure to prevent this complication⁵.
The other options are not correct because:
a) Hyperemesis gravidarum is not an indication for RhIG administration. Hyperemesis gravidarum is a condition where the mother experiences severe nausea and vomiting during pregnancy, which can cause dehydration, electrolyte imbalance, and weight loss. Hyperemesis gravidarum does not affect the blood type or compatibility of the mother and the baby, and does not increase the risk of RhD isoimmunization or HDN.
b) Rh-positive blood test results are not an indication for RhIG administration. Rh-positive blood test results mean that the mother has the RhD antigen on her red blood cells, and therefore she cannot develop antibodies against it¹². Rh-positive mothers do not need RhIG, as they are not at risk of RhD isoimmunization or HDN¹².
d) Anemia is not an indication for RhIG administration. Anemia is a condition where the mother has a low level of hemoglobin or red blood cells, which can cause fatigue, weakness, and shortness of breath. Anemia can have various causes, such as iron deficiency, bleeding, or infection. Anemia does not affect the blood type or compatibility of the mother and the baby, and does not increase the risk of RhD isoimmunization or HDN.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Heart rate is one of the vital signs that reflects the health and well-being of a newborn. It is measured by counting the number of heart beats per minute, either by listening to the chest with a stethoscope or by feeling the pulse at the wrist, elbow, or groin. Heart rate can vary depending on the newborn's activity level, temperature, and emotional state¹.
The normal range for heart rate in full-term newborns is 120 to 160 beats per minute. The heart rate may be slightly higher or lower depending on the newborn's age, weight, and gestational age. For example, premature newborns may have a higher heart rate than term newborns, and heavier newborns may have a lower heart rate than lighter newborns¹².
A heart rate that is too high (tachycardia) or too low (bradycardia) can indicate a problem with the newborn's heart function, oxygenation, or circulation. Some of the possible causes of abnormal heart rate in newborns are:
- Congenital heart defects: structural abnormalities of the heart that are present at birth and affect the blood flow through the heart and the body. They can cause cyanosis (bluish skin color), murmur (abnormal heart sound), poor feeding, or failure to thrive¹³.
- Arrhythmias: irregular or abnormal heart rhythms that can affect the electrical impulses that control the heartbeat. They can cause palpitations (feeling of skipped or extra beats), dizziness, fainting, or cardiac arrest¹³.
- Hypoxia: lack of oxygen in the blood or tissues that can affect the brain and other organs. It can be caused by respiratory distress, anemia, infection, or birth asphyxia. It can cause bradycardia, apnea (pauses in breathing), seizures, or coma¹⁴.
- Hypothermia: low body temperature that can affect the metabolism and organ function. It can be caused by exposure to cold environment, infection, or prematurity. It can cause bradycardia, lethargy, poor feeding, or hypoglycemia (low blood sugar)¹⁴.
- Sepsis: severe infection that can affect the whole body and cause inflammation and organ damage. It can be caused by bacteria, viruses, fungi, or parasites that enter the bloodstream from the mother, the umbilical cord, or the environment. It can cause tachycardia, fever, chills, poor feeding, or shock¹⁴.
Therefore, the nurse should report a heart rate of 72/min to the provider as an abnormal finding and monitor the newborn for any other signs of distress or illness. The provider may order further tests or treatments to determine the cause and severity of the low heart rate and prevent any complications.
The other findings are not findings that the nurse should report to the provider because they are within the
normal range for full-term newborns:
- a) Respiratory rate 55/min is within the normal range for respiratory rate in full-term newborns. The normal range for respiratory rate in full-term newborns is 40 to 60 breaths per minute. The respiratory rate may vary depending on the newborn's activity level, temperature and emotional state¹².
- b) Blood pressure 80/50 mm Hg is within the normal range for blood pressure in full-term newborns. The normal range for blood pressure in full-term newborns is 65 to 95 mm Hg for systolic pressure (the top number) and 30 to 60 mm Hg for diastolic pressure (the bottom number). The blood pressure may vary depending on the newborn's age, weight, and gestational age¹².
- c) Temperature 36.5°C (97.7°F) is within the normal range for temperature in full-term newborns. The normal range for temperature in full-term newborns is 36.5°C to 37.5°C (97.7°F to 99.5°F). The temperature may vary depending on the newborn's activity level, clothing, and environment¹².
Correct Answer is C
Explanation
Cytomegalovirus (CMV) is a common virus that belongs to the herpes family. Most people who get infected with CMV have no symptoms or only mild symptoms, such as fever, fatigue, or sore throat. However, CMV can cause serious problems in newborns who are infected before birth or around the time of birth. This is called congenital CMV infection¹.
Congenital CMV infection can affect various organs and systems in the newborn, such as the brain, eyes, liver, spleen, lungs, and blood. Some of the possible signs and symptoms of congenital CMV infection are:
- Low birth weight
- Small head size (microcephaly)
- Enlarged liver and spleen (hepatosplenomegaly)
- Yellow skin and eyes (jaundice)
- Purple skin patches or bleeding spots (petechiae or purpura)
- Pneumonia
- Seizures
- Inflammation of the brain (encephalitis) or eye (retinitis)
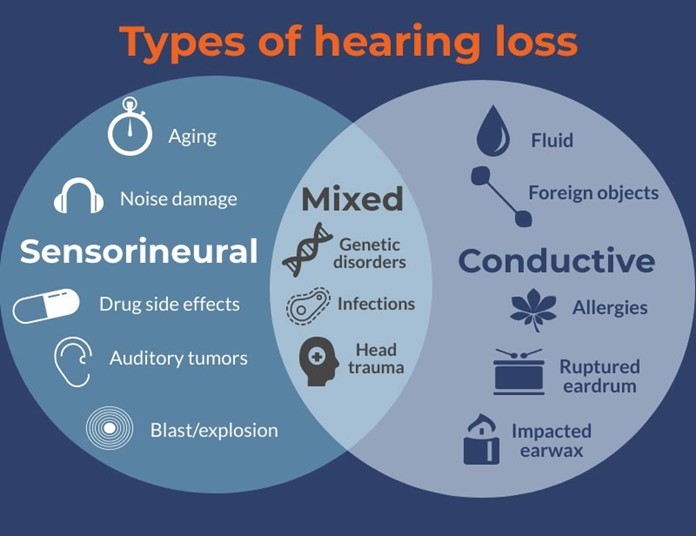
One of the most common and serious complications of congenital CMV infection is hearing loss. Hearing loss can affect one or both ears and can range from mild to profound. Hearing loss can be present at birth or develop later in childhood. Hearing loss can affect the child's speech, language, and cognitive development².
Hearing loss due to congenital CMV infection is often progressive, meaning that it can worsen over time. Therefore, newborns who are diagnosed with congenital CMV infection should have regular hearing tests to monitor their hearing status and receive early intervention if needed. Early intervention may include hearing aids, cochlear implants, speech therapy, or sign language².
The other options are not typical signs of congenital CMV infection and have different causes:
a) Macrosomia is a condition in which a newborn has a birth weight above the 90th percentile for their gestational age. It can be caused by maternal diabetes, obesity, genetics, or prolonged pregnancy.
b) Cataracts are cloudy areas in the lens of the eye that impair vision. They can be caused by genetic disorders, infections, trauma, or exposure to certain drugs or radiation.
d) Urinary tract infection is an infection of the bladder, urethra, kidneys, or ureters. It can be caused by
bacteria, viruses, fungi, or parasites.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
