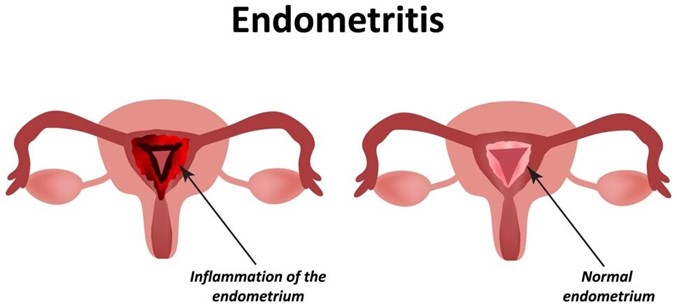
A nurse is assessing a client who is 6 hours postpartum and has endometritis. Which of the following findings should the nurse expect?
Temperature 37.4°C (99.3°F)
Scant lochia
Uterine tenderness
WBC count 9,000/mm³
The Correct Answer is C
Endometritis is an infection of the endometrium, the lining of the uterus, typically occurring after childbirth. When assessing a client with endometritis, the nurse should expect to find uterine tenderness as a common clinical finding. This finding is consistent with endometritis, which is characterized by inflammation and infection of the endometrium. Additional signs and symptoms may include an elevated temperature, increased lochia, foul-smelling lochia, and an elevated WBC count. Prompt identification and treatment of endometritis are important to prevent further complications.
Option a) A temperature of 37.4°C (99.3°F) is within the normal range and does not necessarily indicate endometritis. However, an elevated temperature above 38°C (100.4°F) or a persistent fever may be indicative of an infection and should be further evaluated.
Option b) Scant lochia (minimal vaginal bleeding) is not a characteristic finding of endometritis. In endometritis, lochia is often increased in amount and may have an unpleasant odor.
Option d) A white blood cell (WBC) count of 9,000/mm³ is within the normal range. However, in cases of endometritis, there is usually an elevation in the WBC count as a response to the infection. An elevated or increasing WBC count may be observed.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
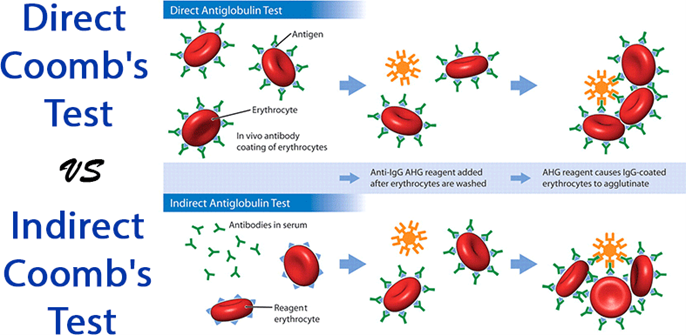
Correct Answer is D
Explanation
An indirect Coombs' test, also known as an indirect antiglobulin test, is used to detect antibodies in your bloodstream that could attach to red blood cells¹². It is used as a screening process to see how you'll react to a blood transfusion². An indirect Coombs' test is also routinely given as part of prenatal testing to see if you have antibodies against Rh-positive blood¹. If you have an Rh-negative blood type and your baby has an Rh-positive blood type, then your immune system could make antibodies that attack your baby's red blood cells¹. This can cause a condition called Rh disease, which can lead to anemia, jaundice or other serious health problems for your baby¹. The indirect Coombs' test can help prevent or treat this problem by detecting the presence of Rh-positive antibodies in your blood¹².
The other options are incorrect because they describe different tests or purposes:
a) The amount of amniotic fluid around the fetus is measured by an ultrasound scan, not by a blood test.
b) The risk of hypoglycemia (low blood sugar) after birth is assessed by measuring the baby's blood glucose level, not by a maternal blood test.
c) The blood flow in the fetus and placenta is studied by a Doppler ultrasound scan, not by a blood test.
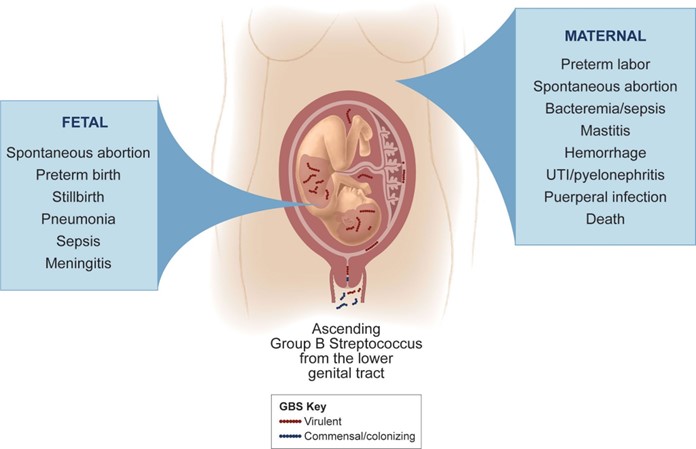
Correct Answer is C
Explanation
Group B Streptococcus β-hemolytic (GBS) is a type of bacteria that can cause serious infections in newborns, such as sepsis, pneumonia, and meningitis. GBS can be transmitted from the mother to the baby during labor and delivery if the mother is colonized with GBS in her vagina or rectum¹.
To prevent GBS infection in newborns, pregnant women who test positive for GBS or have risk factors for GBS should receive intravenous (IV) antibiotics during labor. The antibiotics can reduce the amount of GBS bacteria in the mother's body and lower the chance of passing them to the baby¹².
The recommended antibiotic for GBS prophylaxis is penicillin, which is safe and effective for most women. However, some women may be allergic to penicillin and need an alternative antibiotic. Ampicillin is one of the alternative antibiotics that can be used for GBS prophylaxis in women who have a mild allergy to penicillin (such as rash or itching). Ampicillin is also a type of penicillin, but it has a slightly different structure and may not cause an allergic reaction in some people²³.
Therefore, the nurse should plan to administer ampicillin to the client who tested positive for GBS and has a mild allergy to penicillin. The nurse should also monitor the client for any signs of anaphylaxis (a severe allergic reaction) and have epinephrine ready in case of emergency²³.
The other options are not medications that the nurse should administer to the client:
- a) Cefotetan is another alternative antibiotic that can be used for GBS prophylaxis in women who have a severe allergy to penicillin (such as anaphylaxis or angioedema). However, it is not indicated for women who have a mild allergy to penicillin, as it may still cause cross-reactivity and an allergic reaction²³.
- b) Fluconazole is an antifungal medication that is used to treat fungal infections, such as candidiasis (thrush) or cryptococcal meningitis. It is not effective against bacterial infections, such as GBS, and it is not indicated for GBS prophylaxis⁴.
- d) Doxycycline is an antibiotic that is used to treat bacterial infections, such as chlamydia, gonorrhea, or Lyme disease. It is not effective against GBS and it is not indicated for GBS prophylaxis. Moreover, doxycycline is contraindicated in pregnancy, as it can cause harm to the fetus, such as tooth discoloration or bone growth problems.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
