A client has chest pain rated 8/10 as stated by the patient. The 12-lead ECG reveals ST elevation in the inferior leads and the lab results reveal cardiac enzyme levels are elevated. What is the highest priority for nursing management of this client at this time?
Monitor daily weights and urine output.
Administer TPA to prevent further damage as a result of a clot.
Provide client education on medications and diet to prevent recurrence.
Reduce pain and myocardial oxygen demand.
The Correct Answer is D
A. Monitor daily weights and urine output.
Monitoring daily weights and urine output is an important aspect of managing heart failure or other cardiac conditions. However, in the context of a client with chest pain, ST elevation, and elevated cardiac enzymes (indicating a myocardial infarction), the immediate focus is on addressing the acute event and reducing myocardial oxygen demand.
B. Administer TPA to prevent further damage as a result of a clot.
Tissue plasminogen activator (TPA) is a thrombolytic medication that can be administered to dissolve blood clots in the coronary arteries during a myocardial infarction. However, the administration of TPA has a specific timeframe within which it is most effective. It is crucial to know the elapsed time since the onset of symptoms, and there are specific criteria and contraindications for its use.
C. Provide client education on medications and diet to prevent recurrence.
Client education on medications, lifestyle modifications, and dietary changes is an essential component of long-term management for preventing recurrence of cardiovascular events. However, during the acute phase of a myocardial infarction, the immediate priority is to stabilize the client and address the acute event, with education being a secondary consideration.
D. Reduce pain and myocardial oxygen demand.
During the acute phase of a myocardial infarction, reducing pain and myocardial oxygen demand is the highest priority. This is typically achieved through the administration of medications such as nitroglycerin for vasodilation and opioids for pain relief. Other interventions to optimize oxygen supply and demand, such as supplemental oxygen and reperfusion strategies, may also be considered.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
A. Obtain a sputum sample:
This option is more relevant when the client is experiencing cough with sputum production, which might suggest respiratory issues. However, in the context of coughing after eating or drinking, the primary concern is likely related to the swallowing process rather than respiratory conditions.
B. Inspect the client’s tongue and mouth:
While inspecting the tongue and mouth is a good practice for assessing oral health, it may not directly address the issue of coughing after eating or drinking, which is more indicative of potential swallowing difficulties.
C. Perform a swallowing assessment:
This is the most appropriate option for the given scenario. A swallowing assessment helps identify any abnormalities or difficulties in the swallowing process, which could contribute to the client's coughing after eating or drinking.
D. Assess the client’s nutritional status:
While assessing nutritional status is important for overall health, it may not directly address the immediate concern of coughing after eating or drinking. Nutritional status assessment is a broader aspect of care.
Correct Answer is C
Explanation
A. Kyphosis and clubbing of the fingers:
Kyphosis refers to an excessive forward curvature of the spine, which is not directly related to diminished breath sounds. Clubbing of the fingers is often associated with chronic respiratory conditions, but it is not directly linked to the finding of diminished breath sounds.
B. Dyspnea and hypoxemia:
Dyspnea (shortness of breath) and hypoxemia (low oxygen levels in the blood) are common symptoms in COPD, but diminished breath sounds may indicate an additional concern, such as pneumothorax or other complications.
C. Sepsis and pneumothorax:
Diminished breath sounds can be a sign of pneumothorax, a condition where air accumulates in the pleural space, leading to lung collapse. Sepsis is a risk in clients with COPD due to the potential for respiratory infections. Monitoring for these complications is crucial.
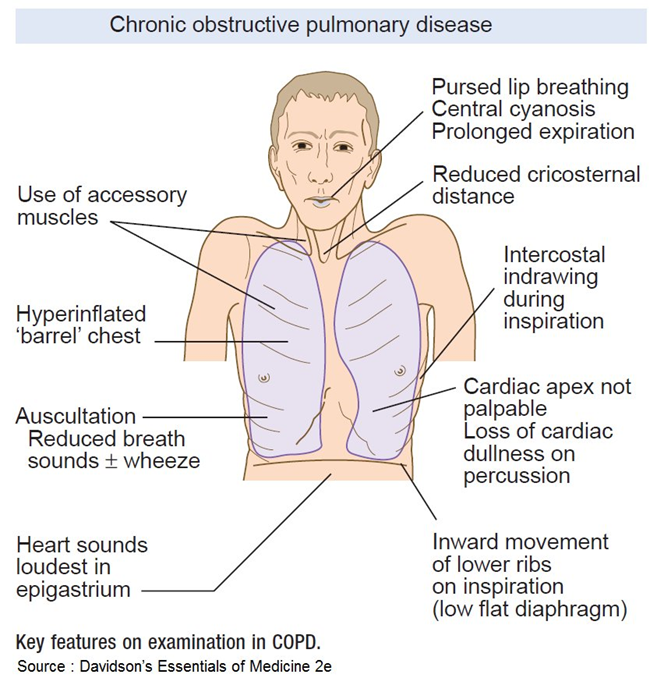
D. Bradypnea and pursed-lip breathing:
Bradypnea (slow breathing) and pursed-lip breathing are coping mechanisms that individuals with COPD may use to manage their breathing difficulties. While they are relevant in the context of COPD, they are not directly associated with the finding of diminished breath sounds.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
