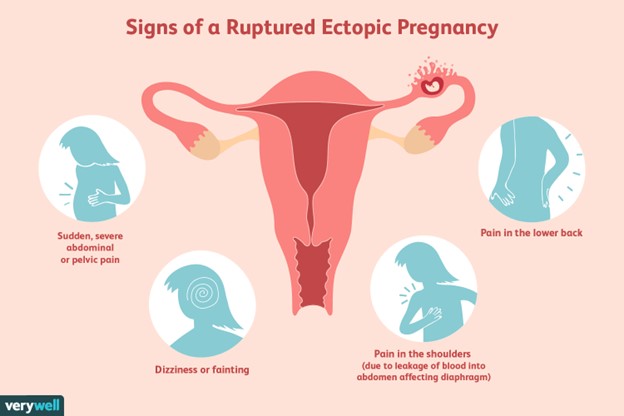
A client is suspected of having a ruptured ectopic pregnancy. Which assessment would the nurse identify as the priority?
Hemorrhage
Edema
Infection
Jaundice
The Correct Answer is A
Choice A reason: Hemorrhage is the most life-threatening complication of a ruptured ectopic pregnancy, as it can lead to hypovolemic shock and death. The nurse should monitor the client's vital signs, blood loss, and level of consciousness, and administer fluids and blood products as ordered.
Choice B reason: Edema is not a common sign of a ruptured ectopic pregnancy, and it is not a priority over hemorrhage. Edema may be caused by other conditions, such as heart failure, kidney disease, or venous insufficiency.
Choice C reason: Infection is a possible complication of a ruptured ectopic pregnancy, but it is not as urgent as hemorrhage. Infection may manifest as fever, chills, malaise, or foul-smelling vaginal discharge. The nurse should administer antibiotics as ordered and monitor the client's temperature and white blood cell count.
Choice D reason: Jaundice is not a typical symptom of a ruptured ectopic pregnancy, and it is not a priority over hemorrhage. Jaundice may indicate liver dysfunction or hemolytic anemia, which are unrelated to ectopic pregnancy. The nurse should assess the client's skin and sclera color, and check the liver enzymes and bilirubin levels.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["A","D","E","F"]
Explanation
Choice A Reason: Homelessness is a risk factor for high-risk pregnancy because it exposes the woman to various challenges and stressors that can affect her health and well-being. Homeless women may face difficulties in accessing adequate nutrition, hygiene, safety, shelter, transportation, and health care. They may also experience higher levels of violence, substance abuse, mental illness, and social isolation. These factors can increase the risk of infections, complications, preterm birth, low birth weight, and infant mortality.
Choice B Reason: Age is not a risk factor for high-risk pregnancy in this case because the woman is 22 years old, which is within the optimal age range for childbearing. The optimal age range is considered to be between 20 and 35 years old, as women in this age group tend to have fewer complications and better outcomes than women who are younger or older. Women who are younger than 20 or older than 35 are considered to have advanced maternal age or adolescent pregnancy, respectively, which are risk factors for high-risk pregnancy.
Choice C Reason: BP 110/70 is not a risk factor for high-risk pregnancy because it is within the normal range for blood pressure. The normal range for blood pressure is considered to be between 90/60 and 120/80 mmHg. Blood pressure that is too high or too low can indicate problems such as preeclampsia, eclampsia, or hypotension, which are risk factors for high-risk pregnancy.
Choice D Reason: BMI 17.5 is a risk factor for high-risk pregnancy because it indicates that the woman is underweight. BMI stands for body mass index, which is a measure of body fat based on height and weight. The normal range for BMI is considered to be between 18.5 and 24.9 kg/m2. BMI that is too low or too high can indicate problems such as malnutrition, obesity, or gestational diabetes, which are risk factors for high-risk pregnancy.
Choice E Reason: Prenatal care is a risk factor for high-risk pregnancy because it indicates that the woman has not received adequate medical attention and support during her pregnancy. Prenatal care is essential for ensuring the health and well-being of both the mother and the baby. Prenatal care involves regular visits to a health care provider who can monitor the progress of the pregnancy, screen for any complications or infections, provide education and counseling, and prescribe any necessary medications or interventions. Lack of prenatal care can increase the risk of maternal mortality, morbidity, preterm birth, low birth weight, congenital anomalies, and infant mortality.
Choice F Reason: Prenatal history is a risk factor for high-risk pregnancy because it indicates that the woman has had previous pregnancies that ended in miscarriage or stillbirth. Prenatal history can provide important information about the woman's reproductive health and potential complications that may recur or affect her current pregnancy. Previous pregnancy losses can indicate problems such as genetic abnormalities, chromosomal disorders, infections, immunological factors, hormonal imbalances, uterine abnormalities, or placental issues. These factors can increase the risk of spontaneous abortion, fetal demise, preterm birth, intrauterine growth restriction (IUGR), or placenta previa.
Correct Answer is {"dropdown-group-1":"D","dropdown-group-2":"C"}
Explanation
Choice A Reason: Preeclampsia is a condition in which a pregnant woman develops high blood pressure and proteinuria (protein in the urine). It can lead to serious complications such as eclampsia, which is seizures caused by preeclampsia, and HELLP syndrome, which is hemolysis, elevated liver enzymes, and low platelets. The main risk factor for preeclampsia is chronic hypertension, which means high blood pressure before pregnancy or before 20 weeks of gestation. Preeclampsia can be detected by measuring the blood pressure and urine protein level. Uric acid is not a reliable indicator of preeclampsia.
Choice B Reason: Gestational diabetes is the correct answer as explained above.
Choice C Reason: Eclampsia is a severe complication of preeclampsia that causes seizures and can be fatal for both the mother and the baby. It usually occurs after 20 weeks of gestation or during labor or postpartum. The main risk factor for eclampsia is preeclampsia, which means high blood pressure and proteinuria during pregnancy. Eclampsia can be prevented by treating preeclampsia with antihypertensive drugs and magnesium sulfate, which is a medication that prevents seizures. Magnesium sulfate can also lower the serum magnesium level, which is the amount of magnesium in the blood. However, magnesium level is not a diagnostic criterion for eclampsia.
Choice D Reason: Placenta previa is a condition in which the placenta covers part or all of the opening of the cervix. It can cause bleeding during pregnancy or delivery and can endanger both the mother and the baby. The main risk factor for placenta previa is previous cesarean section or other uterine surgery, which can cause scarring or damage to the uterine wall. Placenta previa can be detected by ultrasound, which is an imaging test that uses sound waves to create pictures of the uterus and placenta. Hemoglobin is not a relevant factor for placenta previa. Gestational diabetes is a condition in which a woman develops high blood sugar levels during pregnancy. It can cause complications for both the mother and the baby, such as macrosomia, hypoglycemia, and birth trauma. The main risk factor for gestational diabetes is glucose intolerance, which means the body cannot use glucose effectively. Glucose intolerance can be detected by measuring the serum glucose level, which is the amount of glucose in the blood.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
