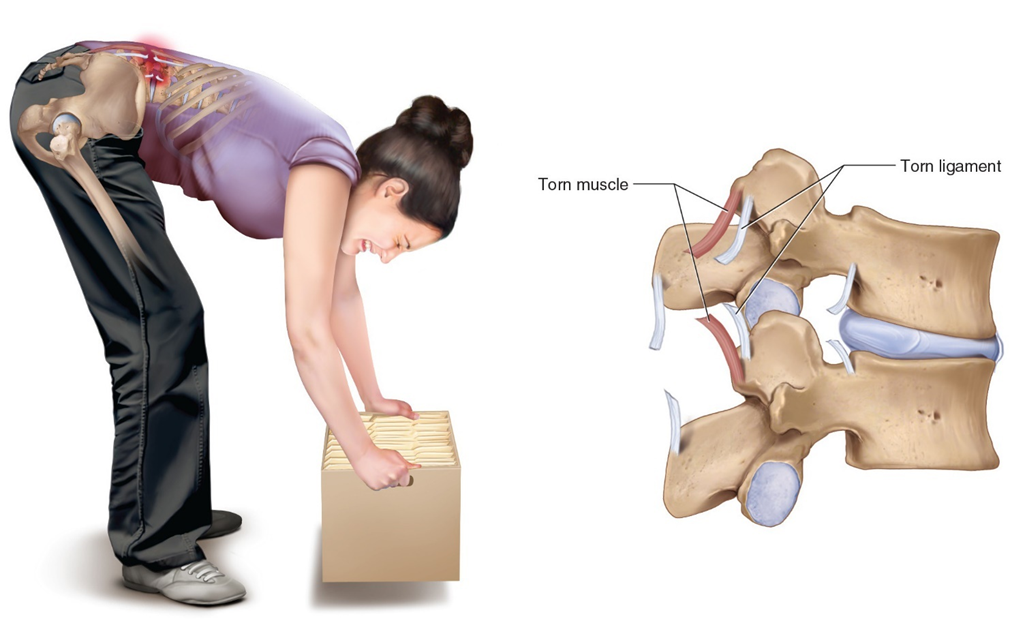
A heating pad is ordered for a patient with a lumbar sprain. The nurse knows that the purpose of the heating pad is to:
Promote healing by increasing the rate of the muscle remodeling process.
Decrease pain by reducing inflammation.
Decrease pain by increasing circulation to a painful area and relaxing tense muscles.
Decrease pain by numbing pain signals.
The Correct Answer is C
Choice A: Promote healing by increasing the rate of the muscle remodeling process
While heat can aid in the healing process by improving blood flow and nutrient delivery to the injured area, it does not specifically increase the rate of the muscle remodeling process. Muscle remodeling involves complex cellular activities that are not solely influenced by external heat application.
Choice B: Decrease pain by reducing inflammation
Heat therapy is generally not used to reduce inflammation. In fact, applying heat to an inflamed area can sometimes exacerbate the inflammation. Cold therapy is more effective for reducing inflammation, especially in the initial stages of an injury.
Choice C: Decrease pain by increasing circulation to a painful area and relaxing tense muscles
This is the correct answer. Applying heat to a painful area causes vasodilation, which increases blood flow and helps deliver oxygen and nutrients to the affected tissues. This process helps to relax tense muscles and alleviate pain. Heat therapy is particularly effective for muscle spasms, stiffness, and chronic pain conditions.
Choice D: Decrease pain by numbing pain signals
Heat therapy does not numb pain signals in the same way that cold therapy does. Cold therapy works by numbing the affected area and reducing nerve activity, which helps to alleviate pain. Heat therapy, on the other hand, works by improving circulation and relaxing muscles.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Choice A reason:
Assessing the operative site is important to monitor for signs of bleeding, infection, or other complications. However, it is not the most critical, high-priority assessment immediately after surgery. While the condition of the surgical site can provide valuable information about the patient’s recovery and potential complications, it does not take precedence over ensuring the patient’s airway is clear and they are breathing adequately. The operative site can be assessed once the patient’s airway, breathing, and circulation are stable.
Choice B reason:
Airway assessment is the most critical, high-priority assessment in the PACU. Ensuring that the patient’s airway is clear and they are breathing properly is paramount because anesthesia can depress the central nervous system, leading to compromised airway patency and respiratory function. The primary goal in the immediate postoperative period is to ensure that the patient is ventilating adequately to prevent hypoxia and other respiratory complications. This involves checking for airway obstruction, monitoring respiratory rate, and ensuring that oxygen saturation levels are within normal ranges (typically 95-100% for healthy individuals). Any issues with the airway must be addressed immediately to prevent life-threatening complications.
Choice C reason:
Assessing the pulse is crucial for monitoring the patient’s cardiovascular status, including heart rate and rhythm. This can help detect arrhythmias, hypovolemia, or other cardiovascular issues that may arise postoperatively. However, while important, it is secondary to ensuring that the patient’s airway is clear and they are breathing adequately. The pulse can be assessed once the airway and breathing are confirmed to be stable. Normal pulse rates for adults typically range from 60 to 100 beats per minute.
Choice D reason:
Assessing skin integrity is important for identifying signs of pressure ulcers, infection, or other skin-related issues. However, this assessment is not the highest priority immediately after surgery. Ensuring the patient’s airway, breathing, and circulation are stable takes precedence. Skin integrity can be assessed once the patient is stable and other critical assessments have been completed. Maintaining skin integrity is essential for overall patient care, but it does not supersede the need to ensure the patient is breathing properly and has a clear airway.
Correct Answer is ["A","B","E","F"]
Explanation
Choice A: All materials that enter the sterile field must be sterile
This is a correct principle of aseptic technique. Ensuring that all materials entering the sterile field are sterile is fundamental to preventing contamination and infection during surgical procedures. Any non-sterile item introduced into the sterile field can introduce pathogens, compromising patient safety.
Choice B: The surgical team working in the operative field must wear sterile gowns and gloves
This is another correct principle. Members of the surgical team who work directly in the operative field must wear sterile gowns and gloves to create a barrier against microorganisms. This practice helps maintain the sterility of the surgical environment and protects both the patient and the healthcare providers.
Choice C: The sterile package is contaminated once it has been opened
This statement is incorrect. A sterile package is not necessarily contaminated once it has been opened, provided it is opened correctly and the contents are handled using aseptic techniques. Proper opening and handling ensure that the sterility of the contents is maintained.
Choice D: The circulating nurse must wear sterile gowns and gloves
This statement is incorrect. The circulating nurse does not need to wear sterile gowns and gloves because they do not work directly in the sterile field. Instead, they assist by providing necessary supplies and support from outside the sterile area.
Choice E: Tables are sterile only at tabletop level. Items extending beneath this level are contaminated
This is a correct principle. In the operating room, the sterility of tables is maintained only at the tabletop level. Any items that extend below this level are considered contaminated and should not be used in the sterile field.
Choice F: A wide margin of safety is maintained between sterile and unsterile fields
This is also a correct principle. Maintaining a wide margin of safety between sterile and unsterile fields helps prevent accidental contamination. This practice ensures that sterile areas remain uncontaminated by non-sterile items or personnel.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
