A nurse in an emergency department is caring for a client who has a sucking chest wound resulting from a gunshot. The client has a blood pressure of 100/60 mm Hg, a weak pulse rate of 118/min, and a respiratory rate of 40/min. Which of the following actions should the nurse take?
Prepare to insert a central line.
Remove the dressing to inspect the wound.
Administer oxygen via nasal cannula.
Raise the foot of the bed to a 90° angle.
The Correct Answer is C
Choice A Reason: This choice is incorrect because inserting a central line is not a priority action for a client who has a sucking chest wound. A central line is a catheter that is inserted into a large vein in the neck, chest, or groin to administer fluids, medications, or blood products. It may be indicated for clients who have hypovolemia, sepsis, or shock, but it does not address the underlying cause of the client's respiratory distress.
Choice B Reason: This choice is incorrect because removing the dressing to inspect the wound may worsen the client's condition. A sucking chest wound is an open wound in the chest wall that allows air to enter and exit the pleural cavity with each breath. This creates a positive pressure in the pleural space that collapses the lung on the affected side and shifts the mediastinum to the opposite side, impairing the ventilation and circulation of both lungs. Therefore, the nurse should apply an occlusive dressing that covers three sides of the wound and allows air to escape but not enter the pleural cavity. Removing the dressing may allow more air to enter and increase the risk of tension pneumothorax, which is a life-threatening complication.
Choice C Reason: This choice is correct because administering oxygen via nasal cannula may help to improve the client's oxygenation and ventilation. A nasal cannula is a device that delivers oxygen through two prongs that fit into the nostrils. It can provide oxygen at low flow rates (1 to 6 L/min) and low concentrations (24 to 44 percent). The nurse should monitor the client's respiratory rate, pulse oximetry, and arterial blood gases to assess the effectiveness of oxygen therapy.
Choice D Reason: This choice is incorrect because raising the foot of the bed to a 90° angle may worsen the client's respiratory distress. This position may increase the pressure on the diaphragm and reduce the lung expansion. It may also decrease the venous return and cardiac output, leading to hypotension and shock. Therefore, the nurse should position the client in a semi-Fowler's position (30 to 45° angle) or high-Fowler's position (60 to 90° angle) to facilitate breathing and prevent further complications.

Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
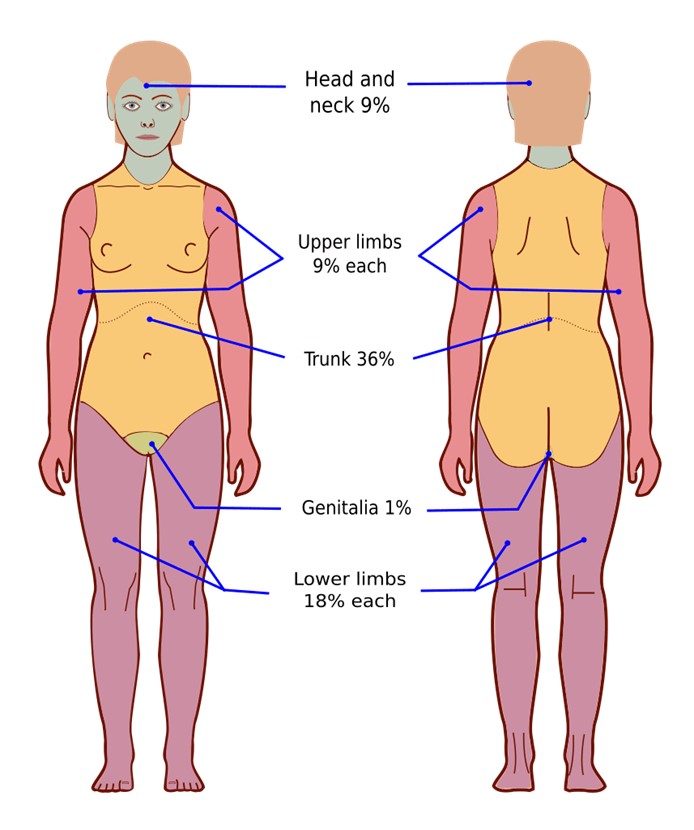
Choice A Reason: Urine output is not a finding that should decrease with adequate fluid replacement. On the contrary, urine output should increase as the fluid therapy restores the renal perfusion and function. The nurse should monitor the urine output and ensure that it is at least 0.5 mL/kg/hr for adults and 1 mL/kg/hr for children.
Choice B Reason: Heart rate is a finding that should decrease with adequate fluid replacement. A high heart rate is a sign of hypovolemia, which occurs when the burn injury causes fluid loss from the intravascular space. The nurse should monitor the heart rate and expect it to decrease as the fluid therapy replenishes the blood volume and improves the cardiac output.
Choice C Reason: Weight is not a finding that should decrease with adequate fluid replacement. On the contrary, weight may increase as the fluid therapy restores the hydration status and corrects the fluid deficit. The nurse should monitor the weight and compare it with the pre-burn weight to evaluate the fluid balance.
Choice D Reason: Blood pressure is not a finding that should decrease with adequate fluid replacement. On the contrary, blood pressure may increase as the fluid therapy restores the vascular tone and improves the tissue perfusion. The nurse should monitor the blood pressure and expect it to increase as the fluid therapy compensates for the fluid loss.
Correct Answer is C
Explanation
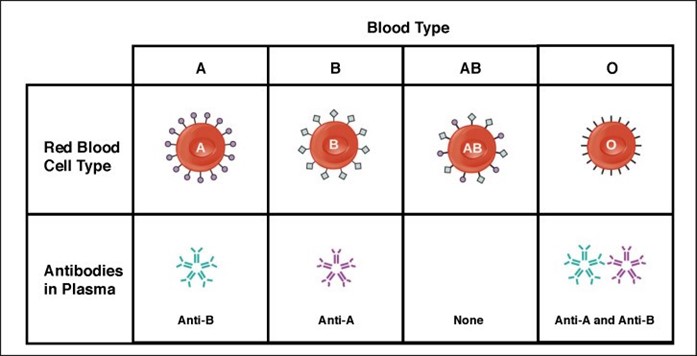
Choice A: Contacting the provider for further orders is not necessary, because the client has type AB blood, which is compatible with any other blood type. The client can receive type B blood without any adverse reactions.
Choice B: Notifying the blood bank of the discrepancy is not required, because there is no discrepancy. The blood bank sent the correct type of blood for the client, according to their blood type.
Choice C: Administering the blood as ordered is the correct action, because type B blood is compatible with type AB blood. The client will not have any transfusion reactions or complications from receiving this type of blood.
Choice D: Completing an incident report is not appropriate, because there is no incident. The nurse did not make any error or mistake in administering the blood to the client. There is no need to document or report anything unusual.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
