A nurse in the emergency room is caring for a client who presents with manifestations that indicate a myocardial infarction. Which of the following prescriptions should the nurse take first?
Attach the leads for a 12-lead ECG.
Initiate oxygen therapy.
Insert the IV catheter.
Obtain a blood sample.
The Correct Answer is B
The correct answer is: B. Initiate oxygen therapy.
Choice A reason:
Attaching the leads for a 12-lead ECG is crucial for diagnosing a myocardial infarction. However, it is not the first priority. Ensuring the patient receives adequate oxygen is more critical to prevent further myocardial damage. The ECG can be performed immediately after oxygen therapy is initiated to confirm the diagnosis and guide further treatment.
Choice B reason:
Initiating oxygen therapy is the first priority because it ensures that the heart muscle receives adequate oxygen, which is essential to prevent further damage during a myocardial infarction. Oxygen therapy helps to maintain tissue oxygenation and can reduce the extent of myocardial injury. This immediate intervention is vital to stabilize the patient and improve outcomes.
Choice C reason:
Inserting the IV catheter is important for administering medications and fluids. However, it is not the first step. Oxygen therapy takes precedence to ensure the heart and other vital organs receive sufficient oxygen. Once oxygen is administered, IV access can be established to facilitate further treatment.
Choice D reason:
Obtaining a blood sample is necessary for confirming the diagnosis and assessing cardiac markers. However, it is not the immediate priority. Ensuring the patient is oxygenated is more urgent to prevent further myocardial damage. Blood samples can be drawn after oxygen therapy is initiated.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice A: Carvedilol is not a medication that interacts with contrast material and places the client at risk for acute kidney injury. Carvedilol is a beta-blocker that lowers blood pressure and heart rate by blocking the effects of adrenaline on the heart and blood vessels. Carvedilol does not affect kidney function or contrast excretion, but it can cause hypotension, bradycardia, or heart failure in some clients.
Choice B: Nitroglycerin is not a medication that interacts with contrast material and places the client at risk for acute kidney injury. Nitroglycerin is a vasodilator that relaxes the smooth muscles of the blood vessels and increases blood flow to the heart. Nitroglycerin does not affect kidney function or contrast excretion, but it can cause hypotension, headache, or flushing in some clients.
Choice C: Atorvastatin is not a medication that interacts with contrast material and places the client at risk for acute kidney injury. Atorvastatin is a statin that lowers cholesterol levels by inhibiting an enzyme that produces cholesterol in the liver. Atorvastatin does not affect kidney function or contrast excretion, but it can cause liver damage, muscle pain, or rhabdomyolysis in some clients.
Choice D: Metformin is a medication that interacts with contrast material and places the client at risk for acute kidney injury. Metformin is an oral antidiabetic drug that lowers blood glucose levels by decreasing hepatic glucose production and increasing insulin sensitivity. Metformin can accumulate in the kidneys and cause lactic acidosis, a life-threatening condition characterized by high levels of lactic acid in the blood. Contrast material can worsen kidney function and increase the risk of lactic acidosis in clients taking metformin. Therefore, metformin should be discontinued before and after the procedure as prescribed.

Correct Answer is D
Explanation
Choice A Reason: This is incorrect because this client has signs of brain death, such as severe head injuries, low respiratory rate, and unresponsiveness. The nurse should tag this client as black, which means deceased or expectant.
Choice B Reason: This is incorrect because this client has non-life-threatening injuries, such as a simple fracture and scratches. The nurse should tag this client as green, which means minor or delayed care.
Choice C Reason: This is incorrect because this client has minor injuries and is able to walk around. The nurse should tag this client as green, which means minor or delayed care.
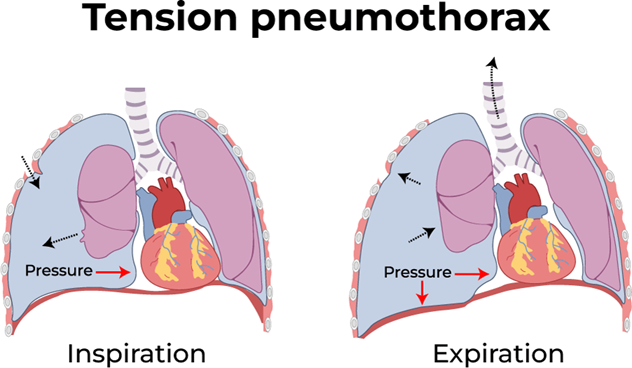
Choice D Reason: This is correct because this client has a life-threatening condition called tension pneumothorax, which requires immediate care. This client has a life-threatening condition called tension pneumothorax, which is caused by air leaking into the pleural space and compressing the lung and the heart. This can lead to respiratory failure, cardiac arrest, and death if not treated immediately. The hissing sound indicates that air is escaping from the lung through the wound. The nurse should tag this client as red, which means immediate care is needed.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
