A nurse is admitting a client who has a partial hearing loss. Which of the following is the priority action by the nurse?
Stand directly in front of the client.
Rephrase statements the client does not hear.
Speak using his usual tone of voice.
Determine if the client uses hearing aids.
The Correct Answer is D
Choice A Reason: This is incorrect because standing directly in front of the client is not the priority action by the nurse when admitting a client who has a partial hearing loss. Standing directly in front of the client can enhance communication, but it is not as important as assessing the client's hearing status and needs.
Choice B Reason: This is incorrect because rephrasing statements the client does not hear is not the priority action by the nurse when admitting a client who has a partial hearing loss. Rephrasing statements can improve understanding, but it is not as essential as evaluating the client's hearing level and preferences.
Choice C Reason: This is incorrect because speaking using his usual tone of voice is not the priority action by the nurse when admitting a client who has a partial hearing loss. Speaking using his usual tone of voice may or may not be appropriate, depending on the client's hearing ability and comfort. The nurse should adjust his tone of voice based on the client's feedback and response.
Choice D Reason: This is the correct choice because determining if the client uses hearing aids is the priority action by the nurse when admitting a client who has a partial hearing loss. Hearing aids are devices that amplify sound and improve hearing for people with hearing loss. The nurse should determine if the client uses hearing aids, and if so, check their function, fit, and battery life. The nurse should also ask about any other assistive devices or strategies that the client uses to communicate effectively.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Choice A Reason: Hemorrhage is not a complication of an acute spinal cord injury, but rather a possible cause of it. Hemorrhage can occur due to trauma or rupture of blood vessels in or around the spinal cord, leading to compression and damage of the nerve tissue.
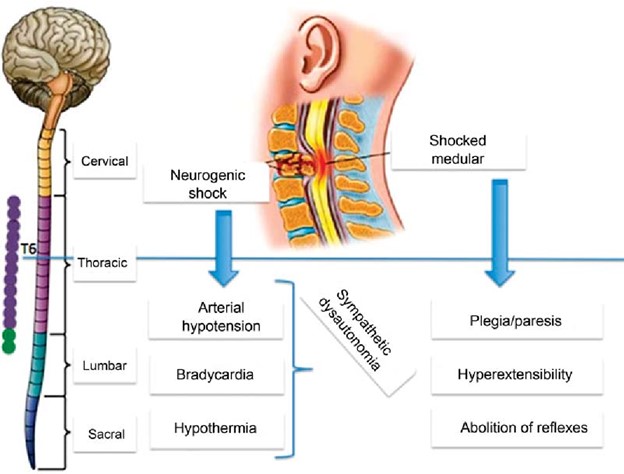
Choice B Reason: This is the correct choice. Spinal shock is a complication of an acute spinal cord injury that occurs within minutes to hours after the injury. It is characterized by loss of sensation, motor function, reflexes, and autonomic function below the level of injury. It is caused by transient disruption of nerve conduction and synaptic transmission in the spinal cord.
Choice C Reason: Apoptosis is not a complication of an acute spinal cord injury, but rather a cellular process that occurs after it. Apoptosis is programmed cell death that occurs in response to injury or stress. It can lead to further loss of neurons and glial cells in the spinal cord over time.
Choice D Reason: Neurogenic shock is a complication of an acute spinal cord injury that occurs within hours to days after the injury. It is characterized by hypotension, bradycardia, and peripheral vasodilation due to loss of sympathetic tone and unopposed parasympathetic activity. It is caused by disruption of autonomic pathways in the spinal cord.
Correct Answer is B
Explanation
Choice A reason: This is incorrect because a drop in heart rate from 74 to 68/min is not a manifestation that requires immediate reporting to the provider. A mild decrease in heart rate can be normal or due to other factors such as medication, sleep, or relaxation. It does not indicate a worsening of brain injury or increased intracranial pressure.
Choice B reason: This is the correct answer because a change in the Glasgow Coma Scale score from 14 to 10 is a manifestation that requires immediate reporting to the provider. The Glasgow Coma Scale is a tool that measures the level of consciousness based on eye-opening, verbal response, and motor responses. A score of 14 indicates mild impairment, while a score of 10 indicates moderate impairment. A decrease in score can indicate deterioration of neurological status and increased intracranial pressure, which can be life-threatening.
Choice C reason: This is incorrect because the headache is not a manifestation that requires immediate reporting to
the provider. Headache is a common symptom of mild TBI and can be managed with analgesics, rest, and hydration. It does not indicate a worsening of brain injury or increased intracranial pressure unless it is severe, persistent, or accompanied by other signs such as vomiting, confusion, or seizures.
Choice D reason: This is incorrect because diplopia is not a manifestation that requires immediate reporting to
the provider. Diplopia means double vision and can be caused by damage to cranial nerves or eye muscles due to TBI. It can be treated with eye patches, glasses, or surgery. It does not indicate a worsening of brain injury or increased intracranial pressure unless it is associated with other symptoms such as blurred vision, loss of vision, or eye pain.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
