A nurse is assessing a newborn who is 4 hr. old. Which of the following findings should the nurse identify as the priority to report to the provider?
Overlapping of the cranial bones
Small, distended white sebaceous glands on the face
Forward and lateral positioning of the ears
Bluish discoloration of the hands and feet
The Correct Answer is D
In a newborn, bluish discoloration of the hands and feet may indicate a condition called peripheral cyanosis, which suggests poor oxygenation. It is important to report this finding to the healthcare provider promptly, as it may indicate a respiratory or circulatory problem that requires immediate attention.
Option a) Overlapping of the cranial bones is a common finding in newborns due to the molding of the head during delivery. This is not a priority finding to report unless there are other signs of concern, such as abnormal head shape or signs of trauma.
Option b) Small, distended white sebaceous glands on the face are called milia and are a normal finding in newborns. They are not a priority finding to report and typically resolve on their own within a few weeks.
Option c) Forward and lateral positioning of the ears is a normal finding in a newborn and is not a priority to report. The ears may appear folded or positioned differently due to the pressure and positioning in the womb.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
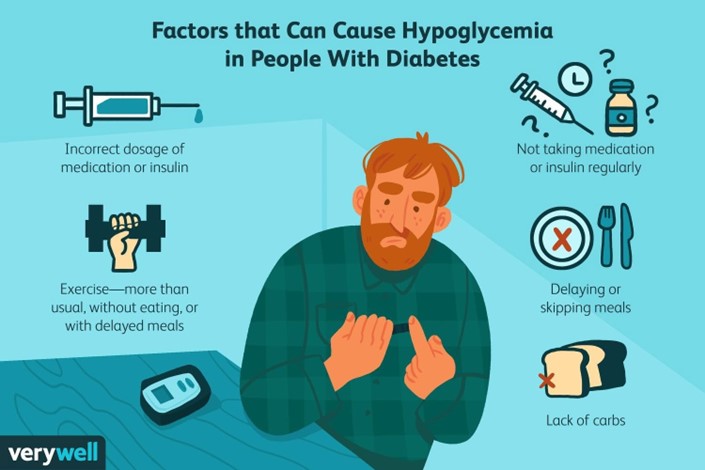
A postpartum client who has type 1 diabetes mellitus and is breastfeeding her newborn should maintain
scheduled mealtimes for herself to prevent hypoglycemia and ensure adequate milk production¹. Breastfeeding may lower glucose levels in the parent and the risk of type 1 and type 2 diabetes in the child¹. Breastfeeding may also help the parent lose weight, prevent diabetes-related complications, and reduce the chances of some cancers¹.
The other options are incorrect because:
a) Taking more insulin with each meal than you did prior to pregnancy may cause hypoglycemia, especially if you are breastfeeding. You should adjust your insulin doses according to your blood glucose levels and carbohydrate intake, and consult your doctor or diabetes educator for guidance²³.
b) Checking your blood glucose levels every 8 hours is not frequent enough to monitor your diabetes during breastfeeding. You should check your blood glucose levels before and after each breastfeeding session, as well as before meals and snacks, at bedtime, and during the night if needed²³.
c) Limiting your carbohydrate intake to 30 grams per day is too restrictive and may impair your milk production and quality, as well as cause hypoglycemia or ketoacidosis. You should consume adequate carbohydrates from healthy sources, such as whole grains, fruits, vegetables, legumes, and dairy products, to meet your energy and nutritional needs²³.
Correct Answer is C
Explanation
A nonstress test (NST) is a test in pregnancy that measures fetal heart rate in response to movement and contractions²³. A normal nonstress test will show a baseline fetal heart rate between 110 and 160 beats per minute with moderate variability (5- to 25-interbeat variability) and 2 qualifying accelerations in 20 minutes with no decelerations³⁴. An acceleration is defined as an increase in the fetal heart rate of at least 15 beats per minute above the baseline for at least 15 seconds²³⁴.
A nonstress test can be affected by uterine contractions, which can cause fetal heart rate decelerations or reduced variability²³. Uterine contractions can also indicate preterm labor or placental abruption, which are serious complications that require intervention². Therefore, if the nurse observes three or more uterine contractions within a 20-minute period during a nonstress test, they should intervene by notifying the provider, assessing the patient for signs of labor or bleeding, and preparing for further evaluation or treatment²⁵.
The other options are not correct because they do not require intervention by the nurse:
a) One acceleration of the FHR within a 20-min period is not enough to meet the criteria for a reactive nonstress test, but it does not indicate fetal distress or compromise. The nurse should continue monitoring the fetal heart rate for another 20 minutes or until two accelerations are observed²³⁴.
b) Uterine contractions lasting 20 to 30 seconds each are normal and expected during pregnancy, especially in the third trimester. They are called Braxton Hicks contractions and they help prepare the uterus for labor. They are usually painless and irregular, and do not cause cervical changes. They do not require intervention by the nurse unless they become frequent, intense, or painful².
d) An FHR that peaks 20 beats above the baseline is considered an acceleration and is a sign of fetal well- being. It does not require intervention by the nurse unless it is associated with decelerations or reduced variability²³⁴.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
